Volume 8 (2025) Issue 1 No.6 Pages 173-180
Abstract
Background: Peri-transplant is a critical period which is associated with a myriad of complications that require pediatric intensive care unit (PICU) referral. PICU outcomes have been historically poor post-hematopoietic stem cell transplantation (HSCT), especially when associated with inotrope support, invasive ventilation, and renal replacement therapy. The study aimed to assess the outcomes of PICU referral in children undergoing HSCT.
Patients & Methods: A retrospective analysis was performed of children between 1 to 18 years of age who underwent HSCT between 2016 to 2023. A clinical deteriorating event (CDE) was defined as an unplanned transfer to the intensive care unit (ICU) or requiring ICU-level intervention on the floor. The reason for PICU referral, place of intervention, cause for the CDE, and requirement of respiratory, renal, and cardiac support were noted. The study period was divided into two 4-year intervals to assess change over time, 2016-2019 and 2020-2023.
Results: In an eight-year period, a total of 934 HSCTs were performed, with 272 patients requiring PICU referral. A total of 415 CDEs were recorded. CDEs for PICU referrals were hypotension (43%), disproportionate tachycardia (42%), respiratory distress (26%), hypertension (22%), altered sensorium (8%), seizures (7.4%), and major bleeds (7.3%). Overall peri-transplant survival was 73.8% (n=201/272). Comparing the two study intervals, 2016-2019 and 2020-2023, the survival of patients on mechanical ventilation had improved from 4.5% to 27.5% (p=0.005) and from 39.4% to 55.9% (p=0.11) among those who received inotropes. Patients with three organ dysfunctions had worse outcomes. Disproportionate tachycardia [OR 0.19 CI 95% (0.06-0.64); p=0.008], hypotension [OR 0.177 CI 95% (0.04-0.84); p=0.029] and acute GVHD [OR 28.46 CI 95% (3.66-221); p=0.001] were significant risk factors for peri-transplant mortality as per multivariate analysis.
Conclusion: Integrated care with the PICU team is the first step towards improving survival in these critically ill children. With timely intervention on the floors for CDEs and protocol-driven care in the PICU, we have demonstrated an increase in overall survival over the past four years and would recommend similar team-based care for units catering to children.
Introduction
Hematopoietic stem cell transplantation (HSCT) is a curative option for a wide range of malignant and non-malignant conditions in children1. It is a complex procedure requiring precision and evidence-based practices. Peri-transplant is a critical period where life-threatening events occur due to underlying disorders, neutropenic sepsis, conditioning toxicity, cytokine release syndrome, and acute graft-versus-host disease2. Adept monitoring by the transplant team and nurses will help recognize danger signs and early interventions.
Pediatric intensive care during HSCT for children has a vital role in treating the abovementioned complications3. It is estimated that 15-20% of children require admission to the pediatric intensive care unit (PICU) after HSCT, with mortality rates ranging from 35% to 80% over the last few decades4, 5. Various factors including the requirement of invasive ventilation, renal and cardiac support, and higher PRISM scores have traditionally been associated with poor outcomes in children post-HSCT4. There is a need to audit the data on PICU referrals during the peri-transplant period to help identify those at-risk children in the future for better prognostication and care.
The aim of the study was to assess the peri-transplant outcomes of a pediatric intensive care unit in children undergoing HSCT.
Patients and Methods
A cross-sectional retrospective analysis was performed in children who underwent HSCT for malignant and non-malignant conditions at a tertiary care center from January 2016 to December 2023. All the children between the ages of 0-18 years at the time of transplant and requiring PICU referral were included in the study. Those who did not require a PICU referral were excluded. Demographic and transplant-related details including age, sex, underlying disease, type of donor (matched family donor (MFD), matched unrelated donor (MUD), or haploidentical donor), and time of transplant were noted. The clinical deteriorating event (CDE), place of intervention (on the floor, in the transplant ward, or PICU), cause of CDE, and three organ support (cardiac, renal, and respiratory systems) requirements, namely inotropes, invasive ventilation, and renal replacement therapy (RRT), were recorded. The primary outcome analyzed was the peri-transplant survival in the children requiring intensive care. The risk factors associated with mortality were studied.
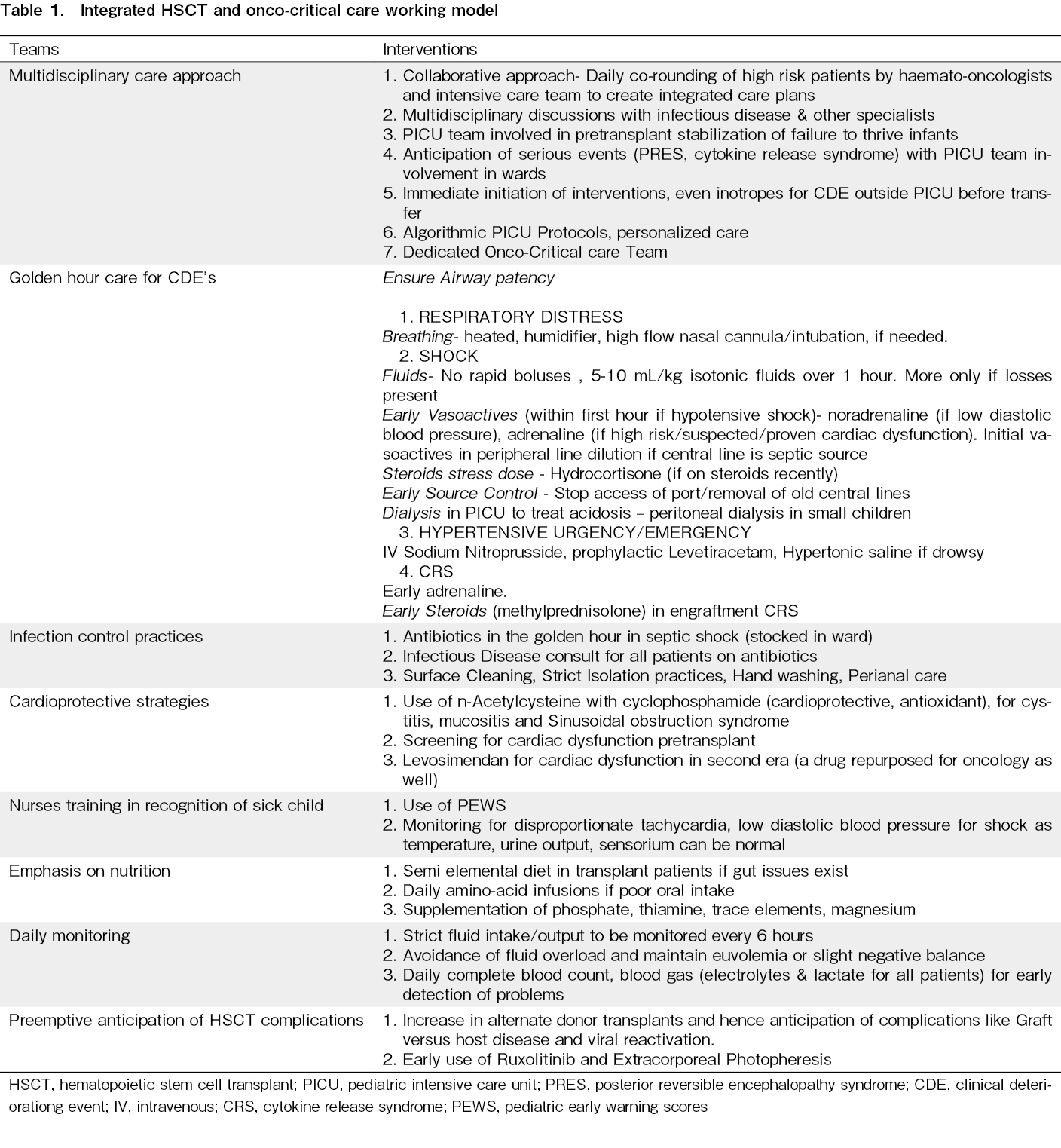
The study period was divided into two 4-year intervals to assess the change over time, 2016 to 2019 and 2020 to 2024. It was after the year 2019 that a dedicated onco-critical care PICU with a seamless working model was established (Table 1). It included a team of full-time pediatric intensivists, clinical intensive care unit (ICU) fellows, and ICU nurses. Prior to 2016, the critical care unit had rotating pediatric intensivists and fellows.
All the PICU referrals in the study warranted PICU admission but because of PICU bed constraints and to avoid delay in
The study has been approved by the institutional review board and ethics approval has been obtained – IEC BMR App No: ASH-C-S-017/07-24. Informed consent has been waived off since it is a retrospective study without identifying individual patient details.
Definitions
CDE was defined as any event that warranted an intensive care unit transfer or ICU-level intervention on the floor. The concept of CDE was adapted from a Latin American study analyzing outcomes of a pediatric oncological unit3, 6. The CDEs analyzed for this study were hypotension, hypertensive urgency, disproportionate tachycardia, seizures, respiratory distress or hypoxia, major bleeding (mucosal) requiring platelet and blood product transfusions, altered sensorium or other central nervous system (CNS) event, and any other.
The peri-transplant period was defined as the time from the commencement of conditioning till Day +30 post-transplant.
Statistical analysis
The above data was collected from the electronic database and patient medical records. The data was entered into predetermined pro forma, collated using a Microsoft Excel sheet, and statistical analysis was performed using IBM SPSS v.28. Descriptive statistics are presented with frequency (percentage). Chi-square/Fisher's exact test was used to determine the association between two independent categorical factors. Univariable and multivariate logistic regression analysis was performed for the outcomes. The multivariable model was performed when a significance was found in the univariate model. A p-value < 0.05 was considered statistically significant.
Results
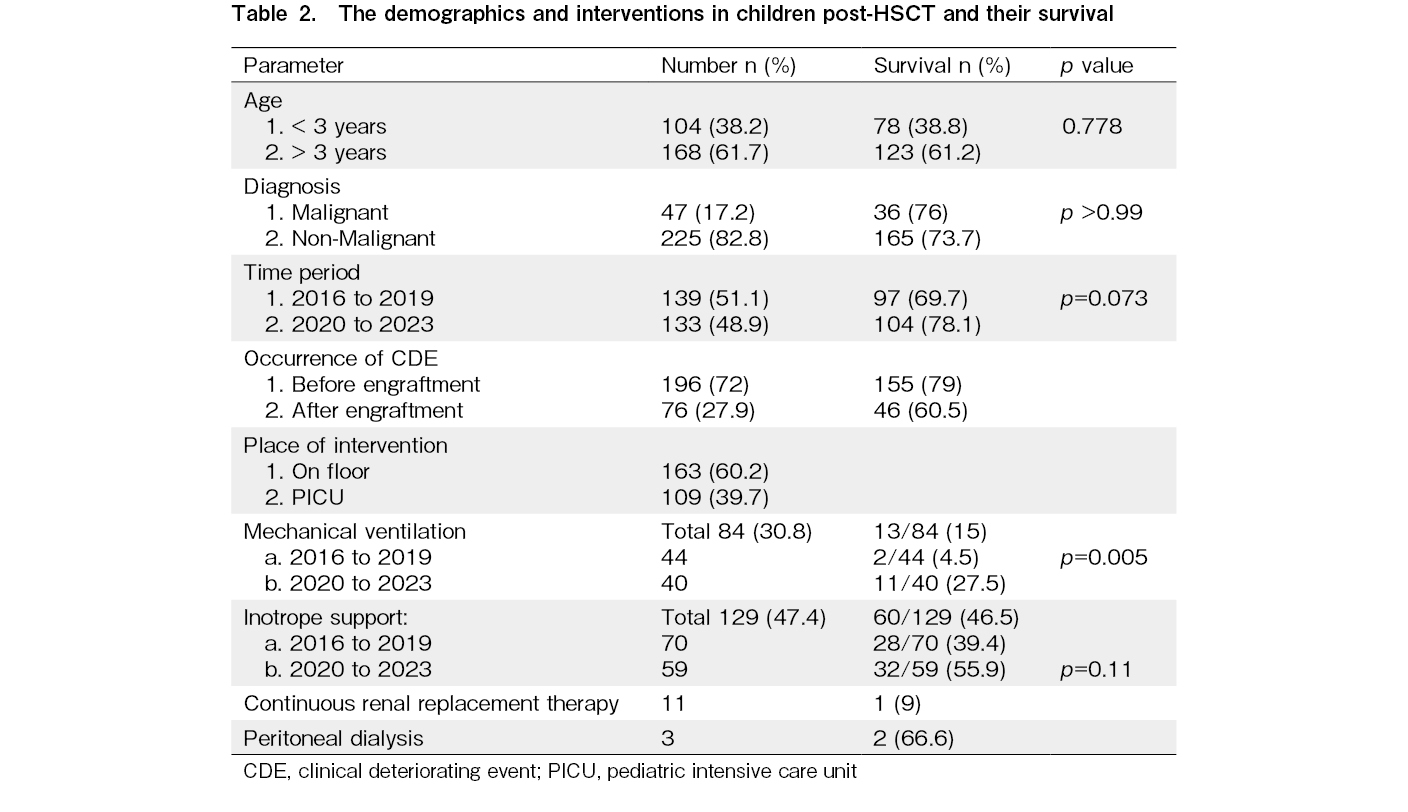
A total of 934 children underwent HSCT in the eight-year period. Of these, 272 (29%) children required PICU referral and were further analyzed (Table 2). The indication for transplant was a non-malignant condition in 225 (82.8%) children and malignant in 47 (17.2%). The donor was MFD in 59 (21.6%), MUD in 52 (19.1%), haploidentical donor in 156 (57.3%), and autologous in 5 (1.8%). The number of transplants were almost equal in both time frames – a total of 139 (51.1%) between 2016-2019 and 133 (48.9%) transplants between 2020-2023.
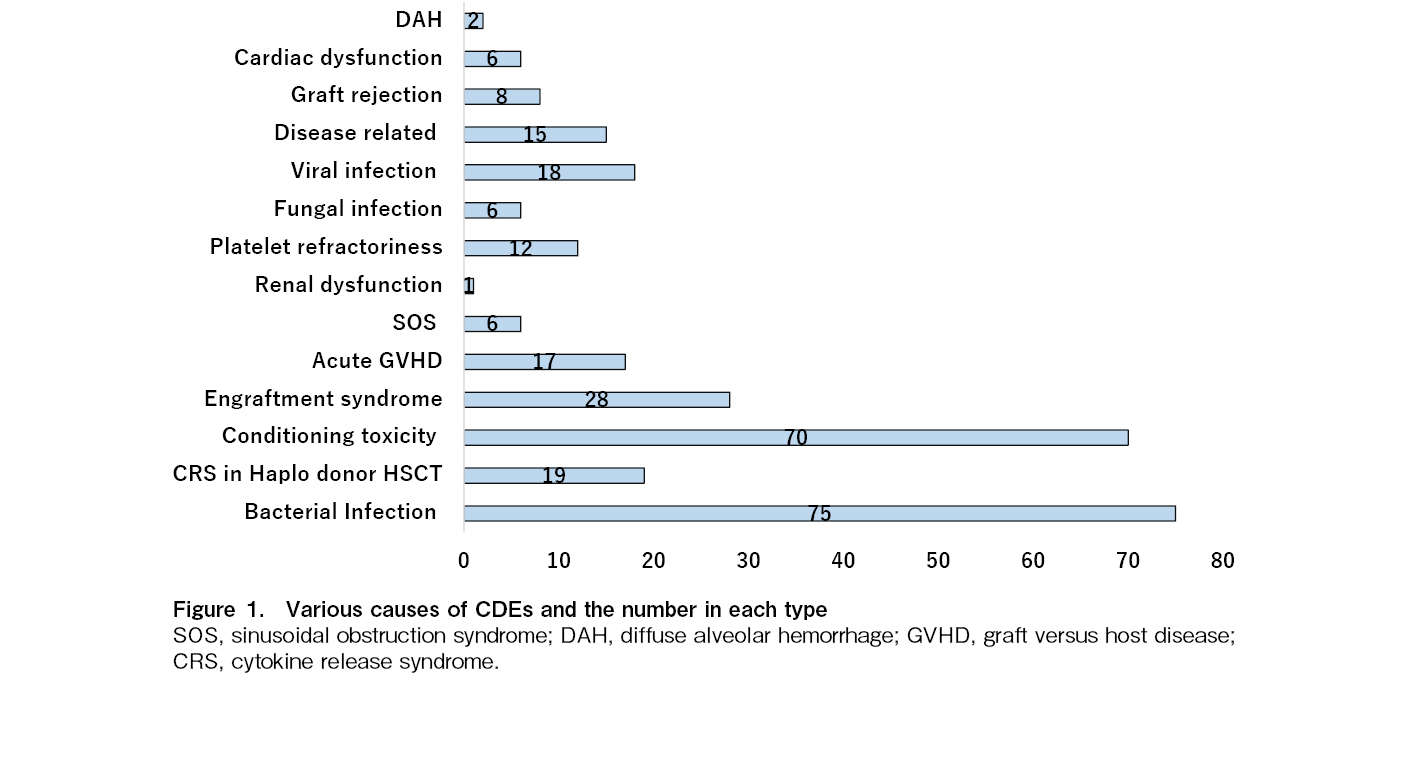
A total of 415 CDEs were recorded in these 272 children. CDEs for PICU referral were hypotension (n=117, 43%), disproportionate tachycardia (n=116, 42%), respiratory distress (n=72, 26%), hypertension (n=60, 22%), altered sensorium (n=22, 8%), seizures (n=14, 7.4%), and major bleeds (n=20, 7.3%). Infections, conditioning toxicity, engraftment syndrome, cytokine release syndrome in haploidentical HSCT, and GVHD (graft-versus-host disease) were the common causes of the CDEs (Figure 1). The place of intervention for the CDEs was on the floor in the transplant ward in 163/272 (60.2%) children, and PICU transfer was required in 109/272 (39.7%) children.
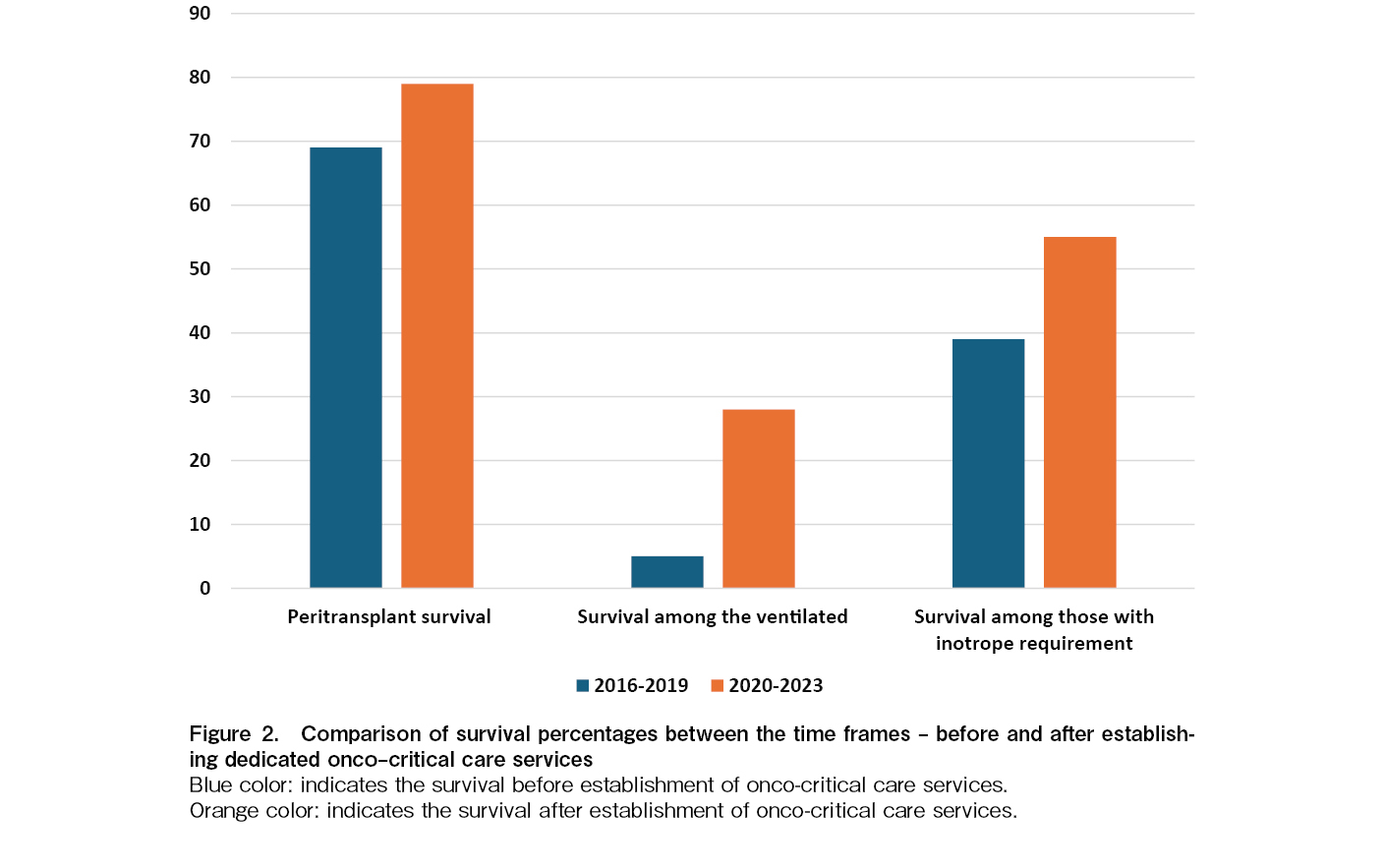
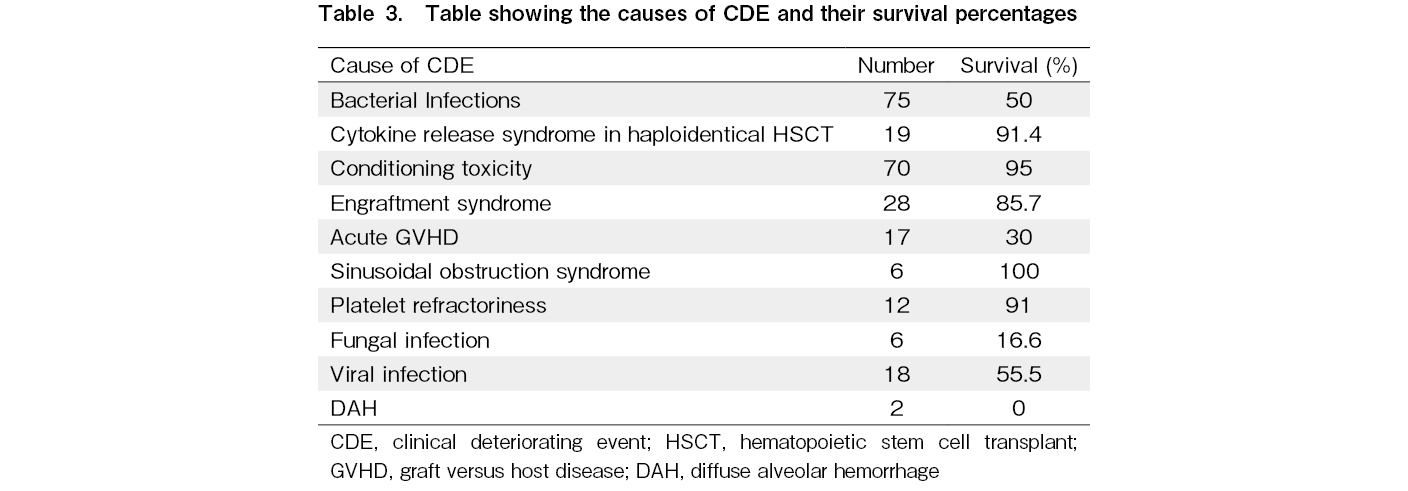
During the peri-transplant period, the overall survival rate in this group was 201 out of 272 (73.8%). When comparing two study periods, 2016 to 2019 and 2020 to 2023, there was an improvement in survival rates from 69% (96 out of 139) to 79% (105 out of 133) (Figure 2). The survival rate was less than 50% in cases of bacterial infections, fungal infections, acute GVHD, and diffuse alveolar hemorrhage. Survival among the various causes of CDE is mentioned in Table 3.
In the univariable analysis, MUD transplants among the donor types, hypotension and disproportionate tachycardia among the CDEs, and bacterial infections and acute GVHD among the causes were associated with poor survival. In the multivariable analysis, hypotension, disproportionate tachycardia, and acute GVHD were associated with poor survival (Table 4). Age, underlying condition, and time of transplant were not significantly associated with peri-transplant survival.
A total of 84/272 (30.8%) needed invasive ventilation, of which 13/84 (15%) were alive at the end of the peri-transplant period. Among these 13 children, 2/44 (4.5%) were transplanted between 2016 to 2019 and 11/40 (27.5%) were transplanted between 2020 to 2023 (p=0.005) (Figure 2).
A total of 129/272 (47.4%) required inotropic support and 60/129 (46.5%) children survived. The survival improved from 28/70 (39.4%) during 2016 to 2019 to 32/59 (55.9%) between 2020 to 2023 (p=0.11) (Figure 2).
Among the children who required renal replacement therapy (RRT), 11 required continuous RRT and only 1 survived (9%) whereas 3 children required peritoneal dialysis, and 2 (66.6%) survived. A total of 13 out of 272 required three organ supports, and 2 of them survived (15.3%).
Discussion
Historically, the survival among children admitted to the ICU after HSCT has been poor due to their immunocompromised state and vulnerable physical condition. A better survival rate is only possible when we identify the signs of deterioration early and provide optimal care as required. When the CDEs were analyzed in this cohort of patients, hypotension, disproportionate tachycardia, and hypertension were the most common. Various infections during the neutropenic state, cytokine storm due to mismatched stem cell infusion, and engraftment syndrome contributed to the numbers of hypotension and disproportionate tachycardia. Hypertension was most likely due to the usage of anti-thymocyte globulin and steroids as part of GVHD prophylaxis.
In this study, 272/934 (29%) children required PICU referral, and a total of 109/934 (11.6%) required PICU transfer. Santhanam et al. from Singapore have shown 18% PICU transfers in children post-HSCT in their eight-year study7. In our cohort, out of the 272 PICU referrals, 60% were treated in the transplant ward providing ICU-level care, and only 40% were shifted to PICU. The ICU-level care provided on the floor in the transplant ward also included inotropes, oxygen support, non-invasive high-flow nasal cannula ventilation, and intense vital monitoring. The Latin American group in pediatric oncology patients showed that 29% of children with CDEs who required ICU-level care were treated on the floor, and most of them eventually had an ICU transfer6. These children requiring ICU-level transfer were treated on the regular floors not intentionally but due to the unavailability of ICU beds at the time of CDE, as in our case.
The overall peri-transplant survival rate of children requiring PICU referral was 73% in this cohort. This includes all the children requiring PICU interventions, those managed on floor and in the PICU. A PICU outcome study from Israel by Zaidman et al. reported a survival rate of 43% post-HSCT8. A multicenter virtual PICU system (VPS) database analysis of 1,782 children post-HSCT requiring PICU intervention from the USA reported an overall mortality of 16.2%, and a combined CIBMTR and VPS analysis in 2020 showed a mortality rate of 17.4%9, 10. An important factor to be noted is that the current analysis included only the peri-transplant period and not all the PICU admissions post-HSCT, unlike the abovementioned multicenter studies. This study adds to the lacunae in literature regarding the peri-transplant PICU outcomes in children.
The present study showed a significant increase in mortality if the donor was a matched unrelated donor, unlike the CIBMTR data, where mismatched unrelated donors had poor outcomes in the univariate analysis10. Among the CDEs, hypotension and disproportionate tachycardia were associated with poor mortality in multivariate analysis, and this sheds light on the importance of regular vitals monitoring in these children. This also emphasizes better training of nurses and trainees in early recognition of warning signs in these children, along with the usage of scales like pediatrics early warning signs11.
The CIBMTR analysis shows no risk of mortality associated with acute GVHD or sinusoidal obstruction syndrome10. In the present cohort of children, the peri-transplant mortality was high when children were admitted into the PICU with acute GVHD and this was in line with the data from the studies by Zaidman et al. and Diaz et al.4, 8. Improved GVHD prophylaxis and early escalation of treatment for GVHD with ruxolitinib and extracorporeal photopheresis will help reduce mortality and morbidity.
Among the infective causes of CDEs, mortality was over 80% in children with fungal infections and close to 50% with viral and bacterial infections. These trends are higher than those from the VPS database study, where the infection-related mortality rate ranged between 22% and 33%9. Poor antibiotic stewardship in the community and the rise of multidrug-resistant bugs are the probable causes for this. The unit's antimicrobial prophylaxis practice included usage of the echinocandin micafungin as an antifungal, intravenous acyclovir as an antiviral, and no prophylactic antibacterials. Post-HSCT viral monitoring with cytomegalovirus, adenovirus, and Epstein-Barr virus DNA-PCRs (polymerase chain reaction) was done once every week from engraftment till day + 100 in haploidentical donor and MUD transplants.
In the present study involving only peri-transplant children, 30.8% of children requiring PICU referral required invasive ventilation, like the USA data9. Invasive ventilation was negatively associated with mortality in most studies, with the mortality in the present cohort being double that of the US cohort9. Among the children who required inotrope support, only half of them survived. Inotrope support was also associated with significant mortality in the study from Zaidman et al.8. Outcomes of children requiring continuous renal replacement therapy were rather dismal, with only 9% survival in the present study, whereas the VPS data analysis from the USA shows 51.9% survival9. Interestingly, outcomes were better when peritoneal dialysis was performed, and 2 out of 3 children survived. This shows early peritoneal dialysis can safely be performed in a select group of children undergoing HSCT.
The outcomes were poor when all three important organs (cardiac, respiratory, and renal systems) were dysfunctional (15.3% survival). Though the survival percentage may vary, this trend was reflected in the multivariate analysis by Santhanam et al., Zaidman et al., the CIBMTR analysis, and in the VPS database cohort7–10.
When the outcomes in the current study were separately analyzed comparing the survival before and after establishing a dedicated PICU for onco-critical care services, the invasive ventilation outcomes were significantly better after 2020, 4.5% to 27.5% (p=0.005). These trends indicate the significant impact a dedicated PICU team can have on children undergoing HSCT and requiring intensive care services. By implementing risk stratification, promptly recognizing critical deterioration events, involving the PICU team early, and intervening on the hospital floors before transfer to modify the course of the illness, we have improved overall survival over the past four years. This improvement can also be attributed to co-rounding by intensivists and oncologists on the wards, close monitoring, and adhering to protocol-driven care in the PICU.
Limitations
The risk factors of mortality for each disease condition were not analyzed individually. Since this was a retrospective study, the analysis did not include in detail the number of children who had ICU-level interventions on the floor before transferring them to the PICU, and objective risk assessment scores like PIM/PRISM were not recorded as well. Hence, a risk predictive score for mortality was not deduced.
Conclusion
Hypotension and tachycardia are the CDEs associated with mortality in multivariate analysis. Invasive ventilation, RRT, and multiorgan failure are associated with poor survival in children post-HSCT, and intervening before irreversible multiorgan failure is the key to successful outcomes. Integrated care with the PICU team is the first step towards improving survival in these critically ill children. We recommend similar team-based care for HSCT units catering to children.
Acknowledgments
We would like to acknowledge the contribution of the infectious disease specialists, stem cell pheresis team, and nursing team in the management of these children.
Author's contribution
The manuscript has been read and approved by all the authors, that the requirements for authorship have been met, and each author believes that the manuscript represents honest work.
ANR, RU, and RR were involved in conceptualizing, data collection, analysis, and manuscript writing. IJ and RM were involved in data analysis and manuscript writing. VM, AN, VVS, and SD were involved in the collection of data and data analysis.
Conflicts of Interest
The authors declare no conflict of interest. Disclosure forms provided by the authors are available on the website.
References
1.Schober S, Huber S, Braun N, Döring M, Lang P, Hofbeck M, et al. Prognostic factors and predictive scores for 6-months mortality of hematopoietic stem cell transplantation recipients admitted to the pediatric intensive care unit. Front Oncol. 2023; 13: 1161573.
2.Michel CS, Teschner D, Schmidtmann I, Theobald M, Hauptrock B, Wagner-Drouet EM, et al. Prognostic factors and outcome of adult allogeneic hematopoietic stem cell transplantation patients admitted to intensive care unit during transplant hospitalization. Sci Rep. 2019; 9: 19911.
3.Agulnik A, Gossett J, Carrillo AK, Kang G, Morrison RR. Abnormal Vital Signs Predict Critical Deterioration in Hospitalized Pediatric Hematology-Oncology and Post-hematopoietic Cell Transplant Patients. Front Oncol. 2020; 10: 354.
4.Diaz MA, Vicent MG, Prudencio M, Rodriguez F, Marin C, Serrano A, et al. Predicting factors for admission to an intensive care unit and clinical outcome in pediatric patients receiving hematopoietic stem cell transplantation. Haematologica. 2002; 87: 292-8.
5.Hume JR, Gupta S, Steiner ME. Historical outcomes of pediatric hematopoietic stem cell transplantation patients requiring critical care. J Pediatr Intensive Care. 2014; 3: 83-90.
6.Agulnik A, Cárdenas A, Carrillo AK, Bulsara P, Garza M, Alfonso Carreras Y, et al. Clinical and organizational risk factors for mortality during deterioration events among pediatric oncology patients in Latin America: A multicenter prospective cohort. Cancer. 2021; 127: 1668-78.
7.Santhanam H, Ong JS, Shen L, Tan PL, Koh PL. Risk Factors for Mortality in Asian Children Admitted to the Paediatric Intensive Care Unit after Haematopoietic Stem Cell Transplantation. Ann Acad Med Singap. 2017; 46: 44-9.
8.Zaidman I, Mohamad H, Shalom L, Ben Arush M, Even-Or E, Averbuch D, et al. Survival of pediatric patients requiring admission in the intensive care unit post hematopoietic stem cell transplantation: Prognostic factors associated with mortality. Pediatr Blood Cancer. 2022; 69: e29549.
9.Zinter MS, Dvorak CC, Spicer A, Cowan MJ, Sapru A. New Insights into Multicenter PICU Mortality Among Pediatric Hematopoietic Stem Cell Transplant Patients. Crit Care Med. 2015; 43: 1986-94.
10.Zinter MS, Logan BR, Fretham C, Sapru A, Abraham A, Aljurf MD, et al. Comprehensive Prognostication in Critically Ill Pediatric Hematopoietic Cell Transplant Patients: Results from Merging the Center for International Blood and Marrow Transplant Research (CIBMTR) and Virtual Pediatric Systems (VPS) Registries. Biol Blood Marrow Transplant. 2020; 26: 333-42.
11.Agulnik A, Mora Robles LN, Forbes PW, Doberanis Vasquez DJ, Mack R, Antillon-Klussmann F, et al. Improved outcomes after successful implementation of a pediatric early warning system (PEWS) in a resource-limited pediatric oncology hospital. Cancer. 2017; 123: 2965-74.
Search
News