Volume 6 (2023) Issue 4 No.6 Pages 139-144
Abstract
Background: Hematopoietic stem cell transplantation (HSCT) has been performed in Singapore since 1985. Currently, more than 100 transplants are performed annually across the public and private sectors. In 2020, the COVID-19 pandemic resulted in unprecedented disruptions to global healthcare systems, and Singapore was no exception. In particular, the field of HSCT faced additional, unique challenges aside from those borne by the healthcare system at large, and appropriate measures were necessary to ensure that HSCT remained available to patients who needed it.
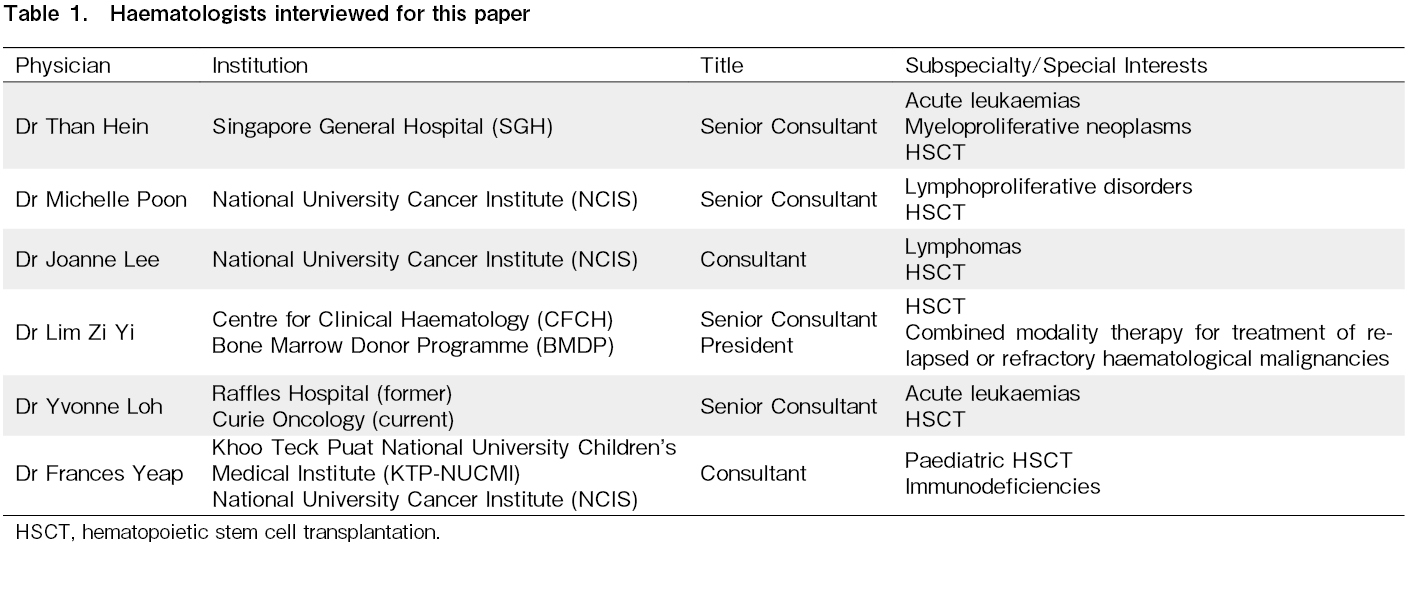
Methods: The expert opinions of six hematologists from various institutions across Singapore were gathered through individual interviews and summarized. This was supplemented by a literature review on bone marrow donation and HSCT in Singapore.
Main Findings and Conclusion: In Singapore, the COVID-19 pandemic has had significant implications for HSCT, ranging from the implementation of additional infection control measures in hospitals to an accelerated rise in haploidentical transplants. Further research is required to better understand and quantify these impacts, improve existing processes, and investigate the effects of COVID-19 and its treatment modalities on patients with HSCT.
Introduction
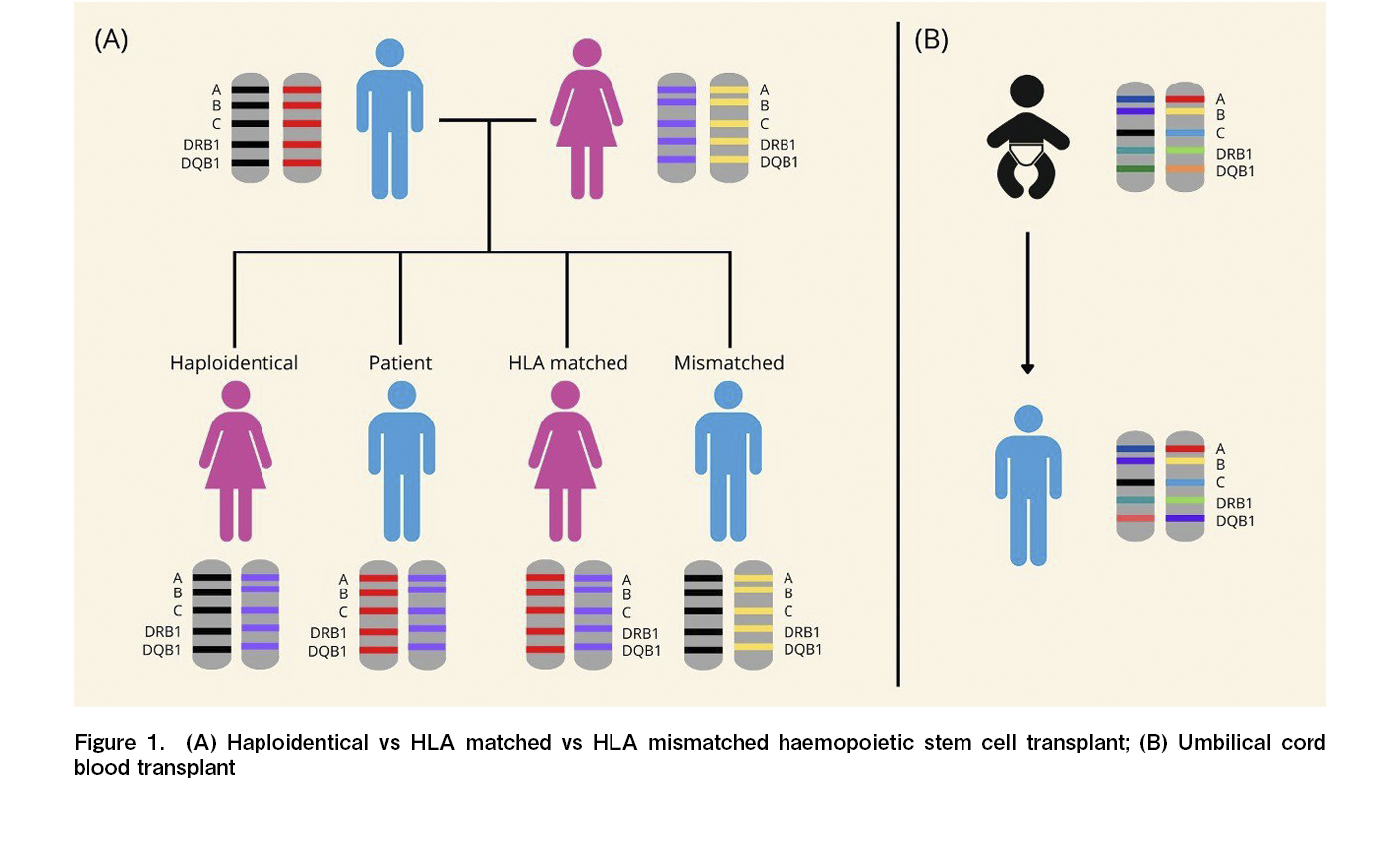
Hematopoietic stem cells (HSC) are harvested, stored, and transplanted to treat various blood disorders. They may be derived from the patient (autologous) or a healthy donor (allogeneic)1. Evolution of the field of HSC transplantation (HSCT) has resulted in safer and more accessible options with diverse HSC sources (Figure 1). International collaborations and organizations, such as the World Marrow Donor Association (WMDA) and the Worldwide Network for Blood and Marrow Transplantation (WBMT), have facilitated Human Leukocyte Antigen (HLA) phenotyping and expanded transplant opportunities for patients worldwide.
The coronavirus disease of 2019 (COVID-19) pandemic had significant adverse impact on HSCT, as it relied on international cooperation and supply chains. The initial period saw a reduction in transplants worldwide due to uncertainty regarding viral transmission and diversion of resources towards infection control2. Beyond logistical concerns, HSCT recipients are known to have significantly higher mortality rates than the general population, possibly due to a newly re-constitutionalized immune system or impaired organ function from treatment-related toxicities3. Therefore, HSCT centers globally were overwhelmed by the pandemic due to difficulties in managing the increased risk and severity of infections4.
Singapore, a small Southeast Asian island nation, has been similarly affected. This paper aims to review the impact of COVID-19 on HSCT protocols and operations in Singapore and identify key gaps in the literature, which include characterizing trends in the use of stem cell sources and describing infection control measures adopted in the context of transplant settings.
Bone marrow donation and transplants in Singapore
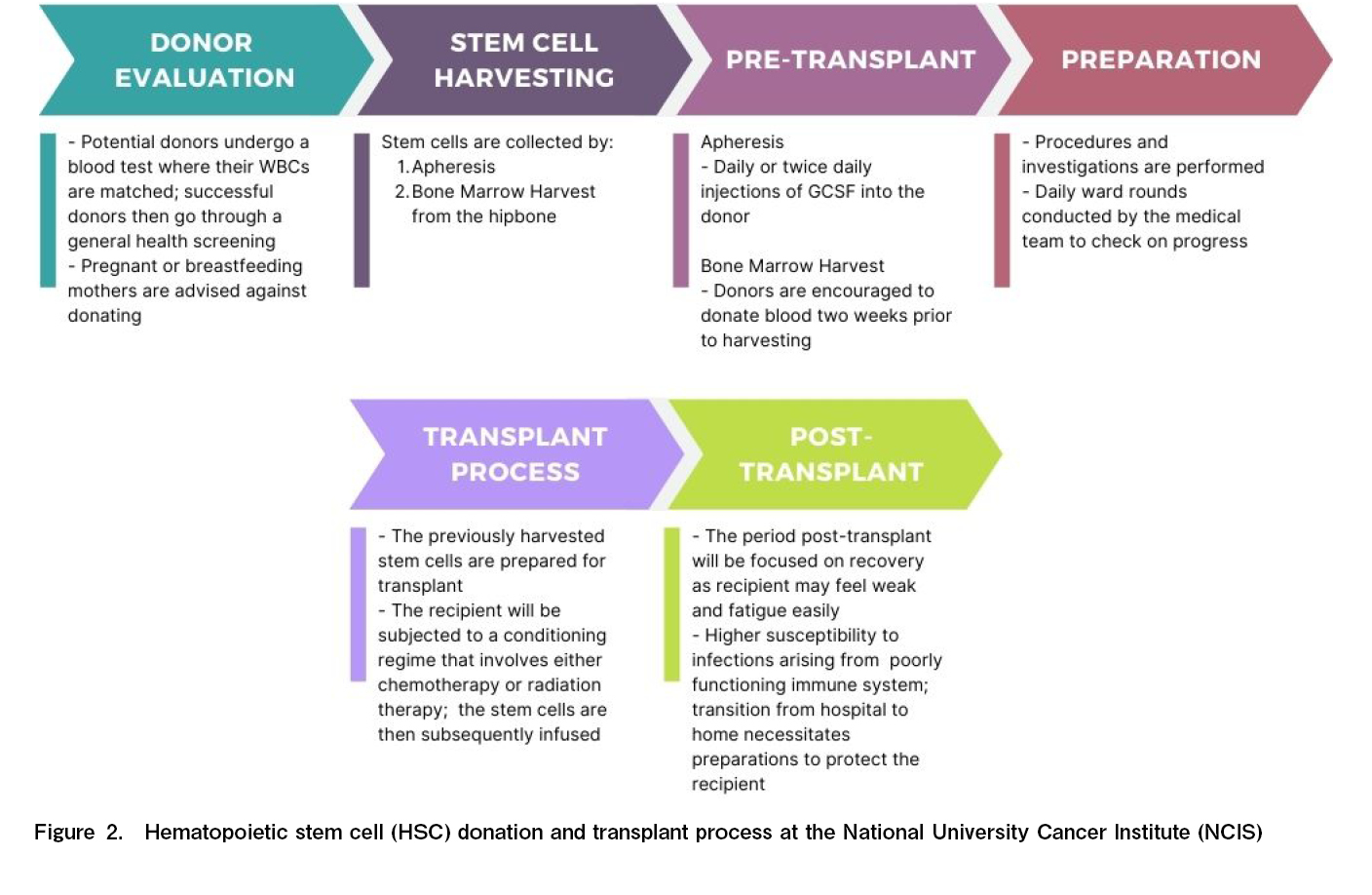
The Bone Marrow Donor Programme (BMDP) maintains Singapore's sole BMD registry. Bone marrow donation is voluntary, with no monetary costs or incentives. Before the pandemic, potential donors underwent a cheek swab test for HLA and blood group analyses, and the results were uploaded to the registry for matching. If a match was found, registered donors were contacted for either peripheral blood stem cell (PBSC) or bone marrow donation, with the latter requiring an overnight hospital stay for observation.
Up to 180 transplants are performed annually in the public and private sectors (
Profiles of the interviewed transplant physicians
We interviewed local transplant physicians from both the public and private healthcare sectors (Table 1) to gain expert insight into how the COVID-19 pandemic has affected HSCT in Singapore.
Singapore's COVID-19 Response
Singapore reported its first COVID-19 case in January 2020. Soon after, the community spread of the virus prompted an escalation in the disease outbreak response system conditions (DORSCON) to orange. Various public health measures were implemented to tackle the outbreak, such as mandatory contact tracing, safe distancing, wearing masks, isolation facilities, and Public Health Preparedness Clinics (PHPCs). A partial lockdown (
HSCT during COVID-19
The challenges faced during the COVID-19 pandemic can be divided into pre, peri, and post transplantation challenges. Pre-transplant concerns included preventing the spread of COVID-19, resource allocation, ensuring the vaccination status of donors, and proper handling of HSCs to prevent blood-borne spread of the virus. Peri-transplant issues included the logistics of receiving foreign donations in Singapore, whereas post-transplant issues involved determining the optimal time for recipient vaccination. Alongside upholding standards of care, supporting patients' socioemotional and psychosocial well-being was essential because of strict isolation protocols. Despite these challenges, Singapore has effectively managed the impact of COVID-19 on HSCT using institutional measures, national pandemic protocols, and a robust healthcare system that enabled patients to continue receiving life-saving grafts safely and feasibly.
Donors
A significant challenge faced by healthcare institutions in Singapore during the pandemic was the availability of donors and the procurement of HSCs, particularly from foreign sources. Travel restrictions and courier service disruptions hindered the usual process of donor travel to Singapore and the prompt delivery of HSCs. Donors had to seek travel approval and undergo quarantine upon arrival, while lockdowns and overwhelmed foreign healthcare systems limited HSC donations. Donor eligibility was also affected by the risk of COVID-19.
To mitigate these challenges, cryopreservation of HSCs from foreign donors has become a routine practice. Additionally, efforts have been made to recruit more local unrelated donors, and alternative sources such as haploidentical donors have been explored for patients lacking HLA-matched options. This ensured a sufficient supply of HSCs for urgent transplants despite limitations in acquiring foreign donor HSCs.
Resource limitations
Resource limitations were a significant concern for healthcare institutions during the pandemic. While there were no widespread shortages of critical supplies, public hospitals faced greater difficulties in resource allocation than the private sector because of higher patient loads. Bed availability for HSCT patients reduced, particularly during the initial stages of the pandemic, as the transplant wards were repurposed as COVID-19 isolation facilities. Securing a single room with proper ventilation and air filters for each patient was logistically challenging. Labor shortages arose as medical staff were redirected to care for COVID-19 patients, leading to a greater workload per capita for transplant teams. In the pediatric setting, resource allocation difficulties were less pronounced because of lower patient volumes compared to adult HSCT. These limitations resulted in delays and necessitated restrictions on the number of transplants performed.
HSC recipients
During the pandemic, the number of patients undergoing HSCT varied across healthcare institutions. Hospitals with a larger proportion of foreign patients experienced approximately a 70% reduction in cases owing to travel restrictions. However, public hospitals handling more local cases experienced relatively unchanged patient loads. The main challenge was the capacity to perform transplants, as various factors such as resource diversion and difficulties in procuring HSCs led many public transplant centers in Singapore to delay or suspend non-urgent transplants. Patients with high-risk conditions such as acute myeloid leukemia and aplastic anemia were likely to undergo HSCT according to the revised COVID-19 protocols. Allogeneic HSCT required additional precautions, whereas stable patients requiring autologous HSCT experienced delays.
In line with the prevailing global consensus, Singapore has avoided unnecessary transplants during the COVID-19 pandemic. However, delays and suspensions in 2020 created a backlog, leading to a surge in transplants in 2021 and making it the busiest year for Singapore's BMDP donor registry to facilitate global transplantation.
PBSC and Alternative Stem Cell Sources
Haploidentical PBSC transplants
The popularity of haploidentical PBSC transplants in Singapore has been on the rise even before the pandemic, similar to the trend of rising haploidentical donors and declining unrelated and sibling donors seen in Europe2. Advancements in haploidentical transplant procedures have made it a viable and cost-effective option with improved treatment outcomes, and an attractive alternative for patients without HLA-matched donors. PBSC collection during the pandemic proved to be challenging; however, harvesting haploidentical donors, most of which were related to recipients, was easier to coordinate and manage than harvesting matched unrelated donors. Therefore, it will remain an important mode of transplantation in the foreseeable future.
Umbilical cord blood
Logistical difficulties and additional control measures made PBSC donation challenging during the pandemic. Consequently, umbilical cord blood (UCB) was expected to prove useful because of a lack of reliance on live donors.
However, most transplanters still prefer PBSC over UCB due to faster recovery and shorter engraftment time7. UCB is also more expensive, requiring two units per adult patient, and lacks lymphocyte integrity for immune recovery post-transplantation. Although fewer UCB transplants are performed in Singapore, it remains a suitable alternative for older patients who may not tolerate haploidentical PBSC transplants. Studies have shown that UCB transplants from unrelated donors are as safe and effective as those from related donors8, highlighting its potential utility in specific cases.
Cryopreservation
Cryopreservation of HSCs allows storage for future use and is commonly used in autologous transplants9. It has also been adopted for allogeneic transplants, extending the window of viability and enabling longer transportation distances. Controlled studies conducted during the pandemic demonstrated that cryopreservation was viable with minimal impact on clinical outcomes10. However, real-world challenges such as stem cell attrition during transit and varying transport times prompted a shift back to fresh transplants in Singapore. Currently, the BMDP only permits cryopreservation of allogeneic transplants when obtaining HSCs from overseas donors.
Infection Control Measures in HSCT
During the COVID-19 pandemic, Singapore's healthcare institutions have implemented additional infection control measures for HSCT donors and recipients. Contact tracing and screening for high-risk donors were performed before transplantation, with donors and recipients undergoing polymerase chain reaction (PCR) tests for COVID-19. Donors required negative tests before HSC mobilization, vaccination at least 2 weeks prior, and negative tests for 9 days before collection. Patients scheduled for HSCT had to take Antigen Rapid Tests (ART) 1-2 times a week, and a positive test delayed conditioning chemotherapy. Visitor restrictions were implemented for all patients, except those on the dangerously ill list (DIL), and staff in the hematology units followed the N95 mask usage and routine COVID-19 testing. The HSCT and infectious disease teams frequently reviewed and adapted standard operating procedures (SOPs) based on the prevailing situation. While SOPs varied between institutions and between the public and private sectors, all hospitals conducted relevant risk assessments and fostered collaboration between HSCT and infectious disease physicians.
During the pandemic, COVID-19 vaccination became an important consideration for transplant patients. While local vaccination rates had little impact on HSCT progression, HSCT is a consideration for vaccination timing. Overseas guidelines, such as the British Society of Blood and Marrow Transplantation (BSBMT)11, recommend vaccinating patients with HSCT 3-6 months post-transplant. Singapore followed similar protocols, with some variations between institutions. Pre-transplant patients were encouraged to receive the standard 2 doses, but the long-term benefits remained questionable, as pre-transplant marrow ablation would eliminate any immunological memory formed in response to the vaccine. Finally, intense pre-transplant treatment hinders vaccination during the peri-transplant period because immunosuppressive drugs may lead to a poorer immune response and reduce vaccine efficacy. Nevertheless, vaccination offers valuable protection against COVID-19.
The post-transplant period is generally more concerning as immunocompromised patients returning to the community are more vulnerable to COVID-19. Therefore, the community incidence of COVID-19 was a key consideration in guiding transplantation decisions. Despite high COVID-19 caseloads, the mortality rate of HSCT patients in Singapore remained below 10%, in contrast to international studies demonstrating a mortality rate as high as 19%4. HSCT patients are more vulnerable than the rest of the Singapore population, with a case fatality rate of 0.1%12.
Future Direction
The pandemic has highlighted HSCT's global interconnectedness, emphasizing the need for partnerships to secure graft access. Continuous investments in healthcare capacity are essential for future pandemic preparedness.
Looking ahead, haploidentical transplants are likely to become the treatment of choice for patients without matched donors, given the increasing evidence of their safety and efficacy.
Conclusion
The COVID-19 pandemic has profoundly affected HSCT in Singapore. Numerous measures have been implemented to mitigate the spread of the virus among HSC donors and recipients while balancing the need to minimize delays. The prevalence of haploidentical transplants continues to rise, accelerated by logistical challenges imposed by the pandemic, and increasing evidence supports it as a viable alternative to fully matched transplants. Additional research is warranted to investigate the impact of COVID-19, vaccination, and the effectiveness of antivirals on HSC recipients as well as novel ways to structure a more resource-efficient HSC procurement process.
Author Contributions
T.L.J.R, G.B and C.Y.H conducted the interviews and wrote the initial manuscript draft. T.H, L.M.M.P and G.Y.T reviewed and edited the paper.
Ethical Approval
No approval from any IRB was required for this review.
Conflicts of Interest
The authors declare no conflict of interest. Disclosure forms provided by the authors are available on the website.
References
1.Majhail NS, Farnia SH, Carpenter PA, Champlin RE, Crawford S, Marks DI, et al. Indications for Autologous and Allogeneic Hematopoietic Cell Transplantation: Guidelines from the American Society for Blood and Marrow Transplantation. Biol Blood Marrow Transplant. 2015; 21: 1863-9.
2.Passweg JR, Baldomero H, Chabannon C, Corbacioglu S, de la Cámara R, Dolstra H, et al. Impact of the SARS-CoV-2 pandemic on hematopoietic cell transplantation and cellular therapies in Europe 2020: a report from the EBMT activity survey. Bone Marrow Transplantation. 2022; 57: 742-52.
3.Sharma A, Bhatt NS, St Martin A, Abid MB, Bloomquist J, Chemaly RF, et al. Clinical characteristics and outcomes of COVID-19 in haematopoietic stem-cell transplantation recipients: an observational cohort study. The Lancet Haematology. 2021; 8: e185-93.
4.Shahzad M, Chaudhary SG, Zafar MU, Hassan MA, Hussain A, Ali F, et al. Impact of COVID-19 in hematopoietic stem cell transplant recipients: A systematic review and meta-analysis. Transplant Infectious Disease. 2022; 24: e13792.
5.Koh MBC, Goh YT, Tan PHC, Koh LP, Hwang WYK, Loh Y, et al. Stem cell transplantation programme at Singapore General Hospital. Bone Marrow Transplantation. 2008; 42: S121-4.
6.Tan JB, Cook MJ, Logan P, Rozanova L, Wilder-Smith A. Singapore's Pandemic Preparedness: An Overview of the First Wave of COVID-19. Int J Environ Res Public Health. 2020; 18: 252.
7.Rocha V, Gluckman E, Eurocord and European Blood and Marrow Transplant Group. Clinical use of umbilical cord blood hematopoietic stem cells. Biol Blood Marrow Transplant. 2006; 12: 34-41.
8.Takahashi S, Ooi J, Tomonari A, Konuma T, Tsukada N, Oiwa-Monna M, et al. Comparative single-institute analysis of cord blood transplantation from unrelated donors with bone marrow or peripheral blood stem-cell transplants from related donors in adult patients with hematologic malignancies after myeloablative conditioning regimen. Blood. 2006; 109: 1322-30.
9.Berz D, McCormack EM, Winer ES, Colvin GA, Quesenberry PJ. Cryopreservation of hematopoietic stem cells. Am J Hematol. 2007; 82: 463-72.
10.Devine S, Kuxhausen M, Spellman SR, Fretham C, Woo Ahn K, Stefanski HE, et al. Cryopreservation of Allogeneic Hematopoietic Cell Grafts Did Not Adversely Affect Early Post-Transplant Survival during the First Six Months of the COVID-19 Pandemic. Blood. 2021; 138 (Suppl 1): 2846.
11.The British Society of Blood and Marrow Transplantation and Cellular Therapy Vaccination Sub-Committee (BSBMT-CT-VSC). SARS-CoV-2 vaccination following haematopoietic stem cell transplant (HSCT) and chimeric antigen receptor Tcell (CAR-T) therapy. updated 31st October 2022, https://www.eviq.org.au/getmedia/ef3f54e6-86aa-49f6-97f6-b8101e0c098e/BSBMTCT-SARS-CoV-2-vaccination-statement-31Oct2022.pdf.aspx [Accessed: 6 June 2023]
12.World Health Organization. Singapore Coronavirus Disease 2019 (COVID-19) Situation Report, 2022, https://www.who.int/singapore/emergencies/covid-19-in-singapore/situation-reports [Accessed: 6 June 2023]
News