Volume 6 (2023) Issue 4 No.2 Pages 114-123
Abstract
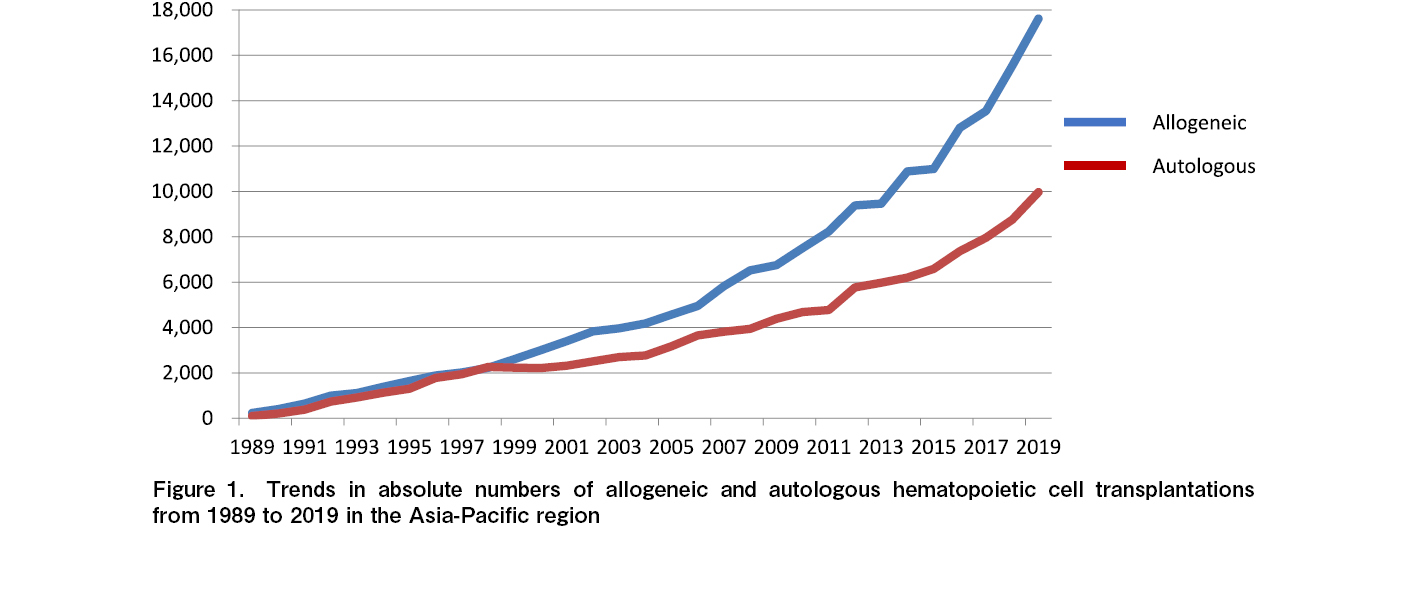
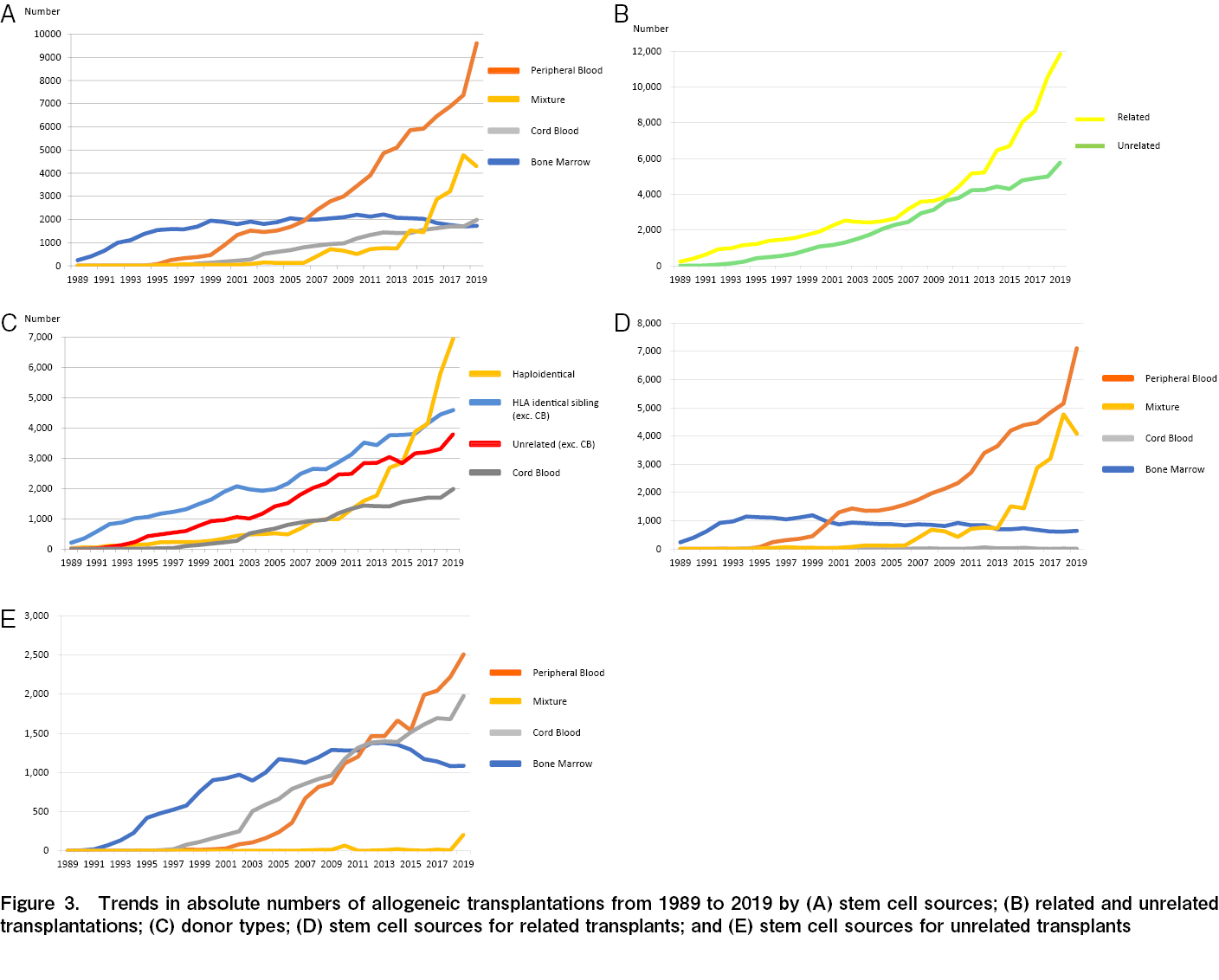
The number of hematopoietic stem cell transplantations (HCTs) is increasing annually worldwide, and the Asia-Pacific (AP) region is no exception. We report on the absolute number of HCTs in 2018 and 2019 and the trends in graft selection and disease indication in the past few decades. In 2018, 24,292 HCTs were performed in the AP region, of which 8,754 (36.0%) were autologous and 15,538 (64.0%) were allogeneic. Among the allogeneic HCTs, 10,552 (67.9%) of the recipients were related to their donors, whereas 4,986 (32.1%) were unrelated. In 2019, 27,583 HCTs were reported, of which 17,613 (63.9%) were allogeneic and 9,970 (36.1%) were autologous. Although, in 2010, there was a nearly equal number of related and unrelated HCTs, the difference has shown an annual increase, with more than double (2.05) the number of related than unrelated HCTs in 2019. Recent trends in the AP region show that peripheral blood has overwhelmingly surpassed the bone marrow as a graft source for both related and unrelated HCTs, with the haploidentical donor type being preferred; however, their trends in each country/region were quite different among countries/regions. In 2019, the main conditions
Introduction
Since the foundation of the Asia-Pacific Blood and Marrow Transplant Group (APBMT) in 1990, we have been collecting hematopoietic stem cell transplantation (HCT) data and assessing the status of HCT in all participating countries/regions annually. The APBMT launched its first Activity Survey in 2007 (collecting the number of HCTs performed in 2005) in seven countries/regions (China, Hong Kong, Iran, Japan, Malaysia, Singapore, and Vietnam). The following year, the Republic of Korea (referred to as South Korea in this paper) and Taiwan participated in the survey. In 2007, Australia and New Zealand joined the APBMT as the Australasian Bone Marrow Transplant Recipient Registry (ABMTRR), and India, Pakistan, the Philippines, and Thailand began to submit data to APBMT. Since 2008, the annual number of HCTs has exceeded 10,000. Centers in Bangladesh, Myanmar, and Sri Lanka began performing HCTs in 2014, Mongolia and Nepal began submitting data to the APBMT Data Center in 2016, and Indonesia reported its first 15 cases in 2018. Nearly 200,000 HCTs were performed between 1986 and 2015 in the Asia-Pacific (AP) region. The first report was published in 20101; this report stated reported the data of 6,418 HCTs that were performed in 432 institutions in nine countries/regions in 2006, and overall, included the data of 58,113 HCTs conducted between 1986 and 2006. Following this, more than 230,000 HCTs were performed in this region. Moreover, with the increase in the number of participating countries/regions and transplants, the transplantation methodology has significantly developed and changed during these past years. APBMT Data Center completed the 15th Activity Survey in 2020, collecting data on the number of HCTs performed in 2019. Here, we aimed to report the absolute numbers of HCTs by disease and graft sources in 2018 and 2019, update all previous data, and revise the trends in graft selection and disease indication over the past few decades.
Materials and Methods
Data collection and definitions
The APBMT Data Center in Japan has been conducting the annual APBMT Activity Survey since 2007. From 2007 to 2018, it collected information regarding the number of transplants in the year 2 years prior; however, since 2018, it began collecting information about the number of transplants performed in the previous year. The original survey sheets are used, and the survey items include disease indication and transplant type. The information was collected through different routes owing to differences in data collection systems among the APBMT participating countries/regions: (1) ABMTRR, Chinese Blood and Marrow Transplantation Registry (CBMTR), Indian Society for Blood and Marrow Transplantation Registry (ISBMT), Korean Society of Blood and Marrow Transplantation (KSBMT), Japan Society for Transplantation and Cellular Therapy (JSTCT)/Japanese Data Center for Hematopoietic Cell Transplantation (JDCHCT), Malaysian Society of Transplantation (MST), and Taiwan Society of Blood and Marrow Transplantation (TBMT), submitted the data on behalf of their countries/regions (Australia, New Zealand, China, India, South Korea, Japan, Malaysia, and Taiwan, respectively). (2) The Ministry of Health and Medical Education of the Islamic Republic of Iran submitted the data from Iran. (3) In Bangladesh, Indonesia, Myanmar, the Philippines, Sri Lanka, and Thailand, individuals responsible for data collection in designated transplant centers merged and submitted their data. (4) Each institution in Hong Kong, Mongolia, Nepal, Pakistan, Singapore, and Vietnam submitted the data individually.
Whenever new participating countries/regions joined the Activity Survey, the data center collected records of the number of transplants conducted in those countries/regions over the past few years. Thus, there was an increase in the total annual number of transplants in the current report compared to our previous reports1–4.
As previously reported3, the APBMT recorded the number of HCTs as two (or more) for a patient who received HCTs twice (or more) per year. Patients who underwent a single procedure of HCT using more than one source of stem cells were recorded as having undergone a mixture of HCTs. These include bone marrow (BM) plus peripheral blood stem cell (PB), BM plus cord blood cell (CB), PB plus CB, and BM plus PB plus CB transplantations.
Transplant facilities
This report counted the number of transplant centers registered in the APBMT Data Center by facility (not department).
The number of transplantations/facilities per population of 10 million
The transplantation rate and facility density in each country/region were calculated as the number of cases of each type of HCT and facilities per 10 million people, respectively. The total population of each country was extracted from the World Bank data5.
Statistical analyses and ethical approval
Every time new countries/regions participated in the Activity Survey, the number of cases recorded from those countries/regions was retrospectively updated, and the results were reanalyzed with the updated data. The APBMT Data Center performed all the necessary analyses for this survey. As the data collected included only the number of HCTs, the Data Center and registries/institutions did not obtain informed consent from each patient. The APBMT Activity Survey was approved by the Institutional Review Board of Aichi Medical University School of Medicine (2022-M003/2022-M004) and the APBMT Registry Committee.
Results
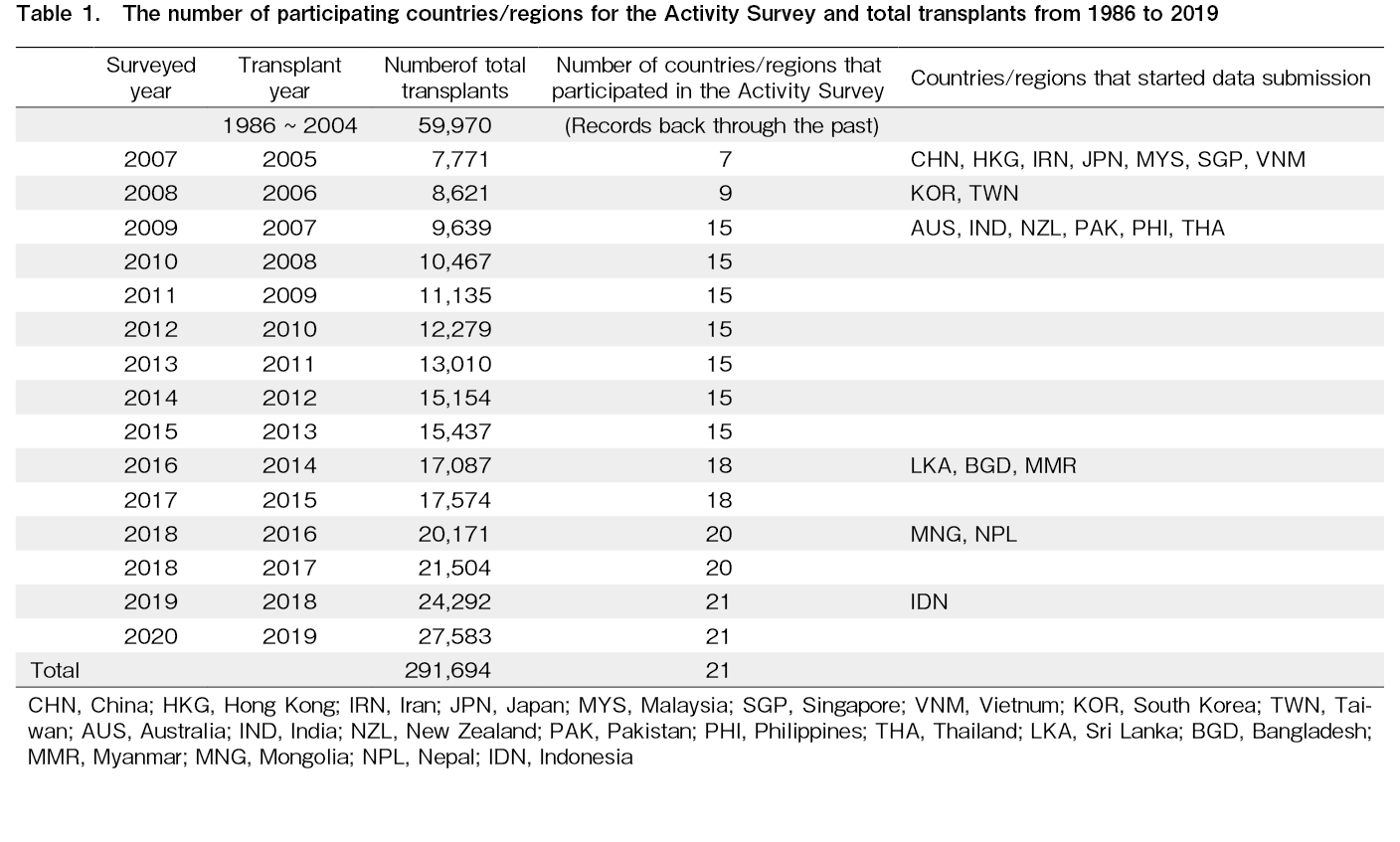
The number of participating countries/regions in the Activity Survey and total transplants from 1986 to 2019 (Table 1)
Overall, seven countries/regions submitted data to APBMT in 2007 (i.e., China, Hong Kong, Iran, Japan, Malaysia, Singapore, and Vietnam), while South Korea and Taiwan began data submission in 2008. In 2009, Australia, India, New Zealand, Pakistan, the Philippines, and Thailand participated in the survey, and the total number of participating countries/regions reached 15. The overall annual transplants exceeded 10,000 in 2008 and 20,000 in 2016. Three countries (Sri Lanka, Bangladesh, and Myanmar), two countries (Mongolia and Nepal), and Indonesia began survey participation in 2016, 2018, and 2019, respectively. Currently, data are collected from 21 countries/regions. We found that the total number of transplants in the AP region has increased annually (291,694 cases in 2019).
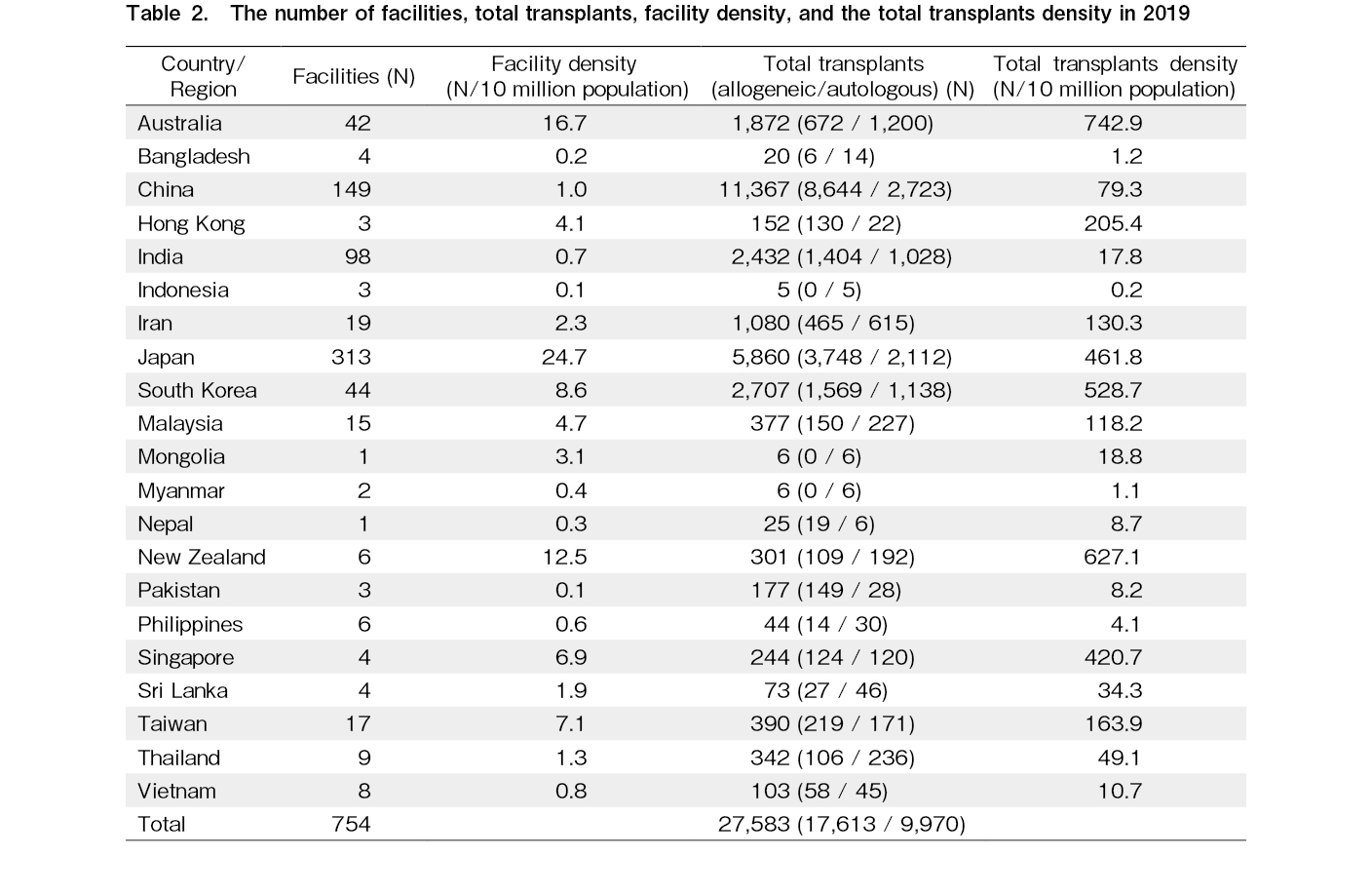
Number of facilities and total transplants in 2019 (Table 2)
In 2019, 27,583 HCTs were performed in the AP region. In China, 11,367 transplants were performed in 2019. This was followed by Japan (5,860), South Korea (2,707), India (2,432), and Australia (1,872). The number of transplants in Iran exceeded 1,000 per year for the first time in 2019 (1,080). In 2008, Indonesia participated in APBMT, and in 2018, they submitted 15 cases of the Activity Survey data. In 2019, they performed five transplantations. When the number of HCTs per transplant facility in each country/region was compared, China had the highest number (76), followed by South Korea (62), Singapore (61), Pakistan (59), and Iran (57). As there are many facilities in Japan (n=313), the number of HCTs per facility was very small (19) despite the very high number of annual transplants. Regarding the number of transplant facilities per 10 million people, Japan had the highest number (24.7), followed by Australia (17.9) and New Zealand (12.5). Conversely, China and India, where the transplant numbers were large, had <1.0 transplant facility per 10 million people because they are the most populated countries worldwide. Many other countries/regions have fewer than one transplant facility per 10 million people, including Bangladesh (0.2), Indonesia (0.1), Myanmar (0.4), Nepal (0.3), Pakistan (0.1), the Philippines (0.6), and Vietnam (0.8). There was also a wide variation in the total number of transplants per 10 million population. New Zealand recorded the highest number (627.1 transplants per 10 million population), while Bangladesh (1.2), Indonesia (0.2), Myanmar (1.1), Nepal (8.7), Pakistan (8.2), and the Philippines (4.1) had <10 transplants per 10 million population.
Stem cell source and donor type
Autologous transplants
In 2019, 9,970 (36.1%) autologous HCTs were reported (
Allogeneic transplantation
In 2019, 17,613 (63.9%) allogeneic HCTs were reported (
Compared with the number of unrelated HCTs, that of related HCTs has increased rapidly since 2010. In 2019, the number of related HCTs (11,839 cases; 67.2%) was approximately twice that of unrelated HCTs (5,774 cases; 32.8%) (Figure 3B and
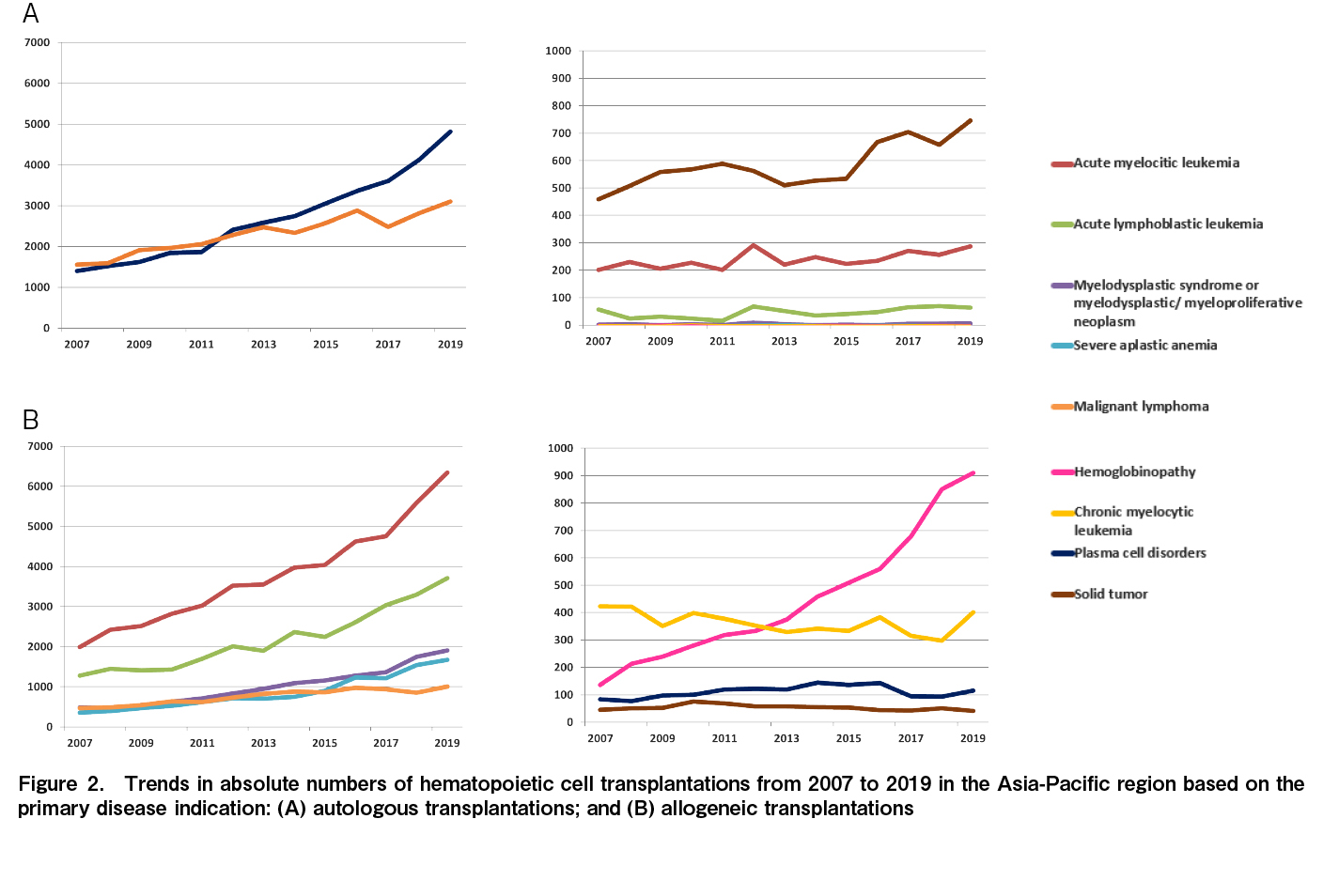
Over the past decade, acute myeloid leukemia (AML) has remained the most common indication for allogeneic HCT, followed by acute lymphocytic leukemia (ALL), myelodysplastic/myeloproliferative neoplasm, and severe aplastic anemia (SAA). The increasing number of transplants for hemoglobinopathy has been significant. It reached 910 HCTs annually in 2019, which was 3.8 times higher than the number of HCTs conducted 10 years ago (Figure 2B,
Trends in donor selection
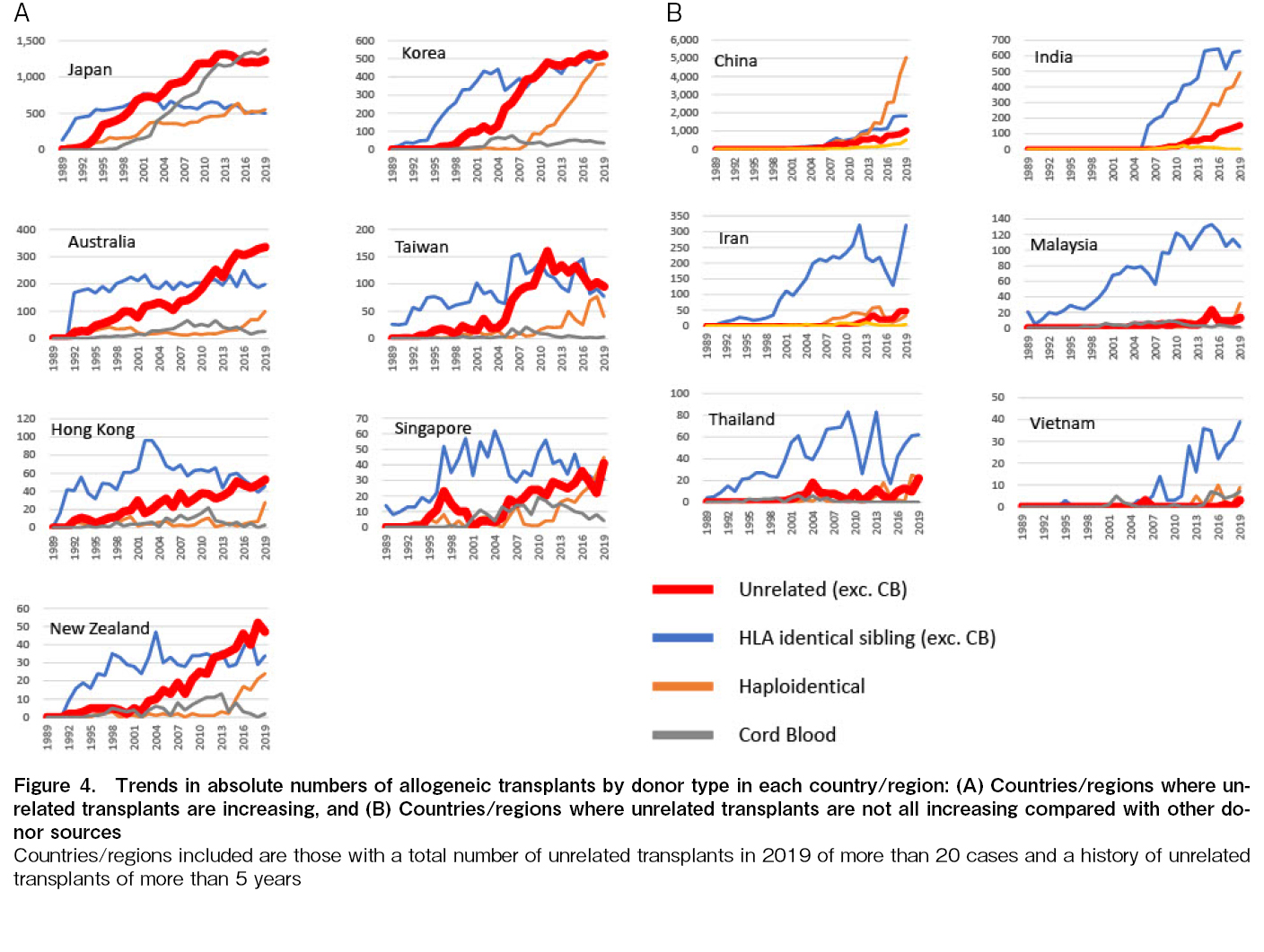
Focusing on the trends of donor selection in countries/regions that continue to perform unrelated transplants (excluding cord blood) as of 2019, we can divide them into two groups. The first group refers to the countries/regions (Japan, South Korea, Australia, Taiwan, Hong Kong, Singapore, and New Zealand) which significantly increased their numbers over the past 10 years compared to other donor sources. In these countries, the number of HLA-identical sibling transplants has been relatively stable since before 2000, and the number of unrelated transplants has been increasing simultaneously (Figure 4A). By contrast, China, India, Iran, Malaysia, Thailand, and Vietnam have presented modest increases in unrelated transplants compared to other donor sources. In these countries, the rise in HLA identical sibling transplantation was dominant, except for China, where haploidentical HCT is rapidly increasing (Figure 4B).
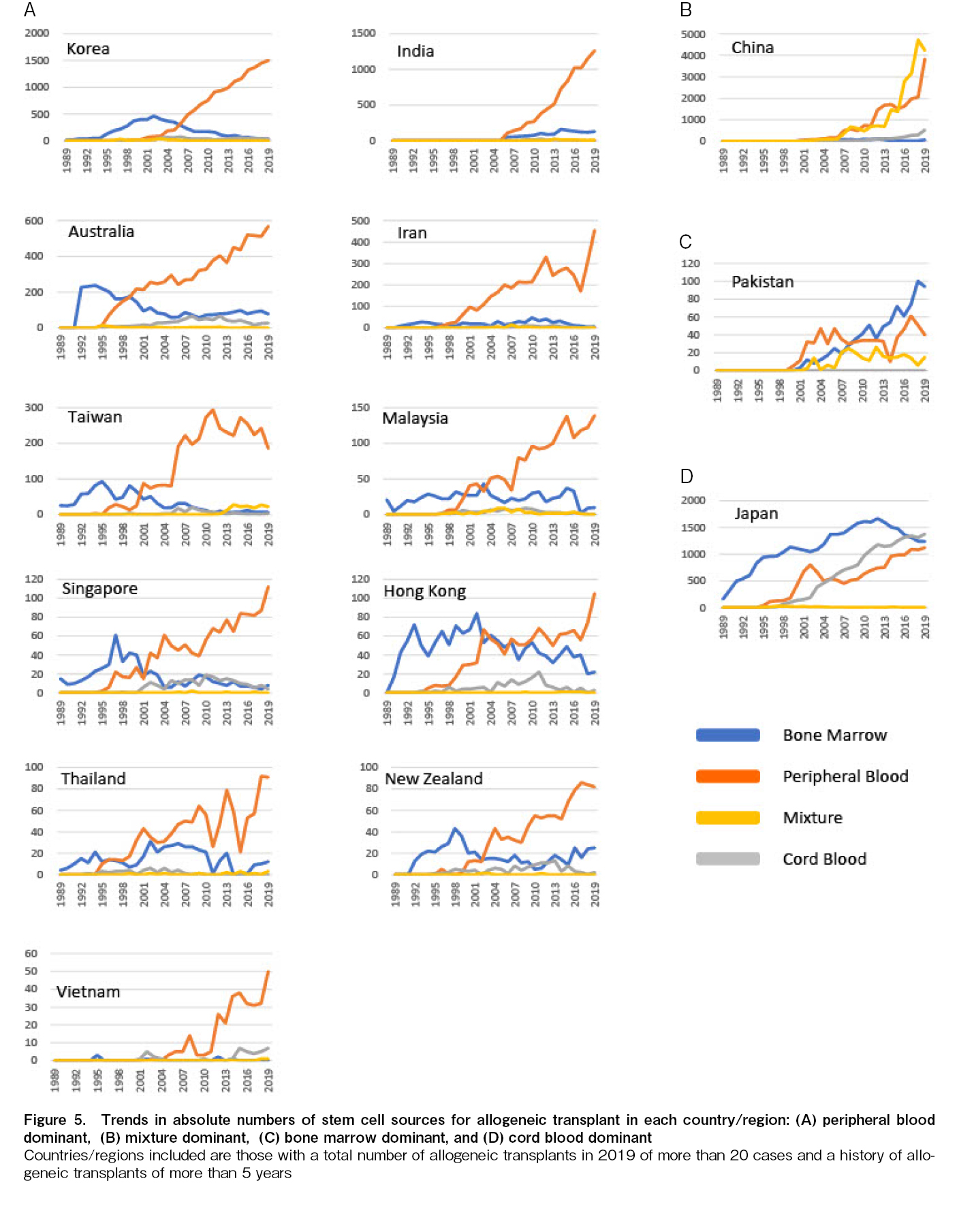
Trends of stem cell source for allogeneic HCT
PB is remarkably dominant in >70% of the countries/regions in this region (South Korea, India, Australia, Iran, Taiwan, Malaysia, Singapore, Hong Kong, Thailand, New Zealand, and Vietnam) for selecting stem cell sources for allogeneic HCT. In these countries/regions, the use of BM has declined over the last decade, while the use of CB has not increased (Figure 5A). China is characterized by the growth in the number of mixture transplants, equivalent to that of PB transplants (Figure 5B). Pakistan and Japan have a higher number of BM than PB transplants; however, Japan is the only country that overwhelms PB and BM with an increased number of CB transplants (Figure 5C and D).
Discussion
This report presents the number of HCT cases in 2018 and 2019 and the trends in HCT sources in the AP region. Yoshimi et al. reported in their first publication that 6,418 HCTs were performed in 432 institutions in 9 countries/regions, and the accumulated number of HCTs between 1986 and 2006 was 58,1131. Since then, the number of countries/regions participating in the Activity Survey has increased by six in 2009, three in 2016, two in 2018, and one in 2019. The number of cases reported from these countries/regions has been retrospectively updated, and this report was reanalyzed with updated data. In 2019, HCTs in this region have continued to increase and exceeded 20,000 cases annually in more than 700 facilities in 21 countries/regions4. The overall number of cases is expected to reach 300,000 in 2020. Compared with our data from 20174, the number of total, allogeneic, and autologous HCTs in 2019 increased by 28.3%, 30.0%, and 25.3%, respectively. Notably, allogeneic HCTs overwhelmed autologous HCTs in this region. Autologous transplants outnumber allogeneic transplants in Europe, the United States, and Latin America6–8. PCD and ML, primarily treated with autologous transplantation, are common in Caucasians, making autologous transplant more prevalent in these regions. Additionally, the abundant reports regarding autologous transplantation and recent emergence of new drugs for these diseases have made transplantation available to patients who were previously ineligible, especially in the economically affluent countries of Europe and in the United States. However, allogeneic transplants have continued to dominate autologous transplants in the AP region over the past 20 years. In contrast to Europe and the United States, in the AP region, the incidence of PCD and ML is relatively low and the reporting rate of the number of autologous HCT might be lower than the actual numbers. Since most APBMT participating countries/regions belong to the world's lower-middle- or upper-middle-income economies5, a delay in responding to expensive new drugs for PCD and ML may occur. Moreover, China and Japan, which are ranked first and second in the number of cases of transplants, performed many haploidentical transplants and unrelated CB transplants, respectively, reflected in the result that allogeneic transplants were more common than autologous transplants.
The total number of HCTs in this region continues to grow, especially in China and India, where growth is unmatched anywhere else worldwide; however, owing to the huge population of the AP region, it is challenging to meet the demand for transplantation in each country/region, and patient access to transplantation has not improved. In fact, 13 countries/regions (Bangladesh, Hong Kong, Indonesia, Mongolia, Myanmar, Nepal, New Zealand, Pakistan, the Philippines, Singapore, Sri Lanka, Thailand, and Vietnam) had fewer than ten transplant facilities, and three countries/regions (Indonesia, Mongolia, and Myanmar) reported <10 transplant cases annually. Only autologous transplants are performed in Indonesia, Myanmar, and Mongolia. Furthermore, as of 2019, Bangladesh, Nepal, Pakistan, and the Philippines have not performed unrelated HCTs. These are lower- to upper-middle-income countries5, and significant effort is required to establish and operate HCT programs in these countries/regions compared to those in high-income countries. Human and financial resources are indispensable for promoting HCT, especially for allogeneic and unrelated HCTs. To this end, efforts are needed at the level of individuals and facilities and to comprehensively promote the following: 1) the establishment of transplant registries, 2) requests for cooperation at national level or among policymakers, 3) education of physicians and health workers, and 4) appeals for available donors. Yeh et al. reported on the launch of a transplant program in Bangladesh with limited resources9 and concluded that it was necessary to systematize and introduce HCT programs in emerging countries by referring to such examples to promote essential transplantation medical care in the very near future. To quickly initiate allogeneic transplants in these countries, the APBMT has provided support for training healthcare professionals in transplant-developing countries at transplant facilities and has formulated center standard guidelines that can be applied to developing countries. It has sent official letters to the Ministry of Health, Labor and Welfare of several countries requesting their cooperation in promoting HCT. It is considered essential to continue these efforts in the future.
We reported the trends in the number of transplants by main disease indications for all transplants and showed that cases of AML, ML PCD, ALL, MDS or MDS/MPN, SAA, and hemoglobinopathy have continuously increased since the 1980s4. In this report, the trends of each disease were analyzed separately for autologous and allogeneic transplantation. In the AP region, PCD, ML, and solid tumors were the main indications for autologous HCTs, and our results were very similar to global trends6. Conversely, the number of autologous HCTs for patients with AML and ALL in this region has increased slightly. This is slightly different from the worldwide trend, wherein, the number of autologous HCTs for acute leukemia is decreasing10. This result directly reflects the fact that a certain number of autologous transplantations for acute myeloid leukemia are performed in China, where most transplantations take place in Asia. Reflecting on the exponential growth of haploidentical HCT, the number of allogeneic transplants has sharply increased in recent years. A particular characteristic of this region is the high rate of allogeneic HCTs by haploidentical donors using a mixed source. It also primarily reflects the increase in haploidentical HCTs in China.
Although the annual Activity Survey data may help in describing the overall trend of HCT in this region and the results are recognized as
Acknowledgments
We sincerely thank all the members of the APBMT, especially the scientific committee members and their data managers, who gathered data from each registry, country, center, and hospital annually. We are also grateful for the cooperation of all participating teams, countries/regions, organizations, and their staff, especially ABMTRR, CBMTR, ISBMT, Ministry of Health and Medical Education of the Islamic Republic of Iran, KSBMT, JSTCT/JDCHCT, MST, and TBMT. This study was conducted by the APBMT Registry Committee and Data Center. We also thank Yukari Nakao and Hiroe Namizaki of the APBMT Data Center for their assistance. All centers that contributed to the Activity Survey reported in this study are listed in
Author Contributions
MI, SO, and YA designed the study, and MI wrote the manuscript. KL, XJH, HH, JHM, YA, AD, LX, BK, AAH, MB, KWH, UB, AH, TF, JS, PCD, MA, WR, MRB, AAG, DS, BSP, KB, KML, and AS submitted the data. MI and APBMT Data Center analyzed the data. All co-authors reviewed the manuscript, and AH, JWL, YK, and SO revised it.
Conflicts of Interest
The authors declare no conflict of interest. Disclosure forms provided by the authors are available on the website.
MI, AS, MB, AAH, and SO are editors of
References
1.Yoshimi A, Suzuki R, Atsuta Y, Iida M, Lu DP, Tong W, et al. Hematopoietic SCT activity in Asia: a report from the Asia-Pacific Blood and Marrow Transplantation Group. Bone Marrow Transplant. 2010; 45: 1682-91.
2.Iida M, Kodera Y, Dodds A, Ho AYL, Nivison-Smith I, Akter MR, et al. Advances in hematopoietic stem cell transplantation in the Asia-Pacific region: the second report from APBMT 2005-2015. Bone Marrow Transplant. 2019; 54: 1973-86.
3.Iida M, Dodds A, Akter M, Srivastava A, Moon JH, Dung PC, et al. The 2016 APBMT Activity Survey Report: Trends in haploidentical and cord blood transplantation in the Asia-Pacific region. Blood Cell Ther. 2021; 4: 20-8.
4.Iida M, Liu K, Huang XJ, Depei W, Kuwatsuka Y, Moon JH, et al. Trends in disease indications for hematopoietic stem cell transplantation in the Asia-Pacific region: A report of the Activity Survey 2017 from APBMT. Blood Cell Ther. 2022; 5: 87-98.
5.The World Bank. Population, total. https://data.worldbank.org/indicator/SP.POP.TOTL [Accessed: April 22, 2023]
6.Niederwieser D, Baldomero H, Bazuaye N, Bupp C, Chaudhri N, Corbacioglu S, et al. One and a half million hematopoietic stem cell transplants: continuous and differential improvement in worldwide access with the use of non-identical family donors. Haematologica. 2022; 107: 1045-53.
7.Passweg JR, Baldomero H, Chabannon C, Basak GW, de la Cámara R, Corbacioglu S, et al. Hematopoietic cell transplantation and cellular therapy survey of the EBMT: monitoring of activities and trends over 30 years. Bone Marrow Transplant. 2021; 56: 1651-64.
8.Auletta JJ KJ, Chen M, Shaw BE. Center International Blood & Marrow Transplantation Research. Current use and outcome of hematopoietic stem cell transplantation: CIBMTR US summary slides, 2021. https://cibmtr.org/CIBMTR/Resources/Summary-Slides-Reports [Accessed: 22 April 2023]
9.Yeh AC, Khan MA, Harlow J, Biswas AR, Akter M, Ferdous J, et al. Hematopoietic stem-cell transplantation in the resource-limited setting: Establishing the First Bone Marrow Transplantation Unit in Bangladesh. Journal of global oncology. 2018; 4: 1-10.
10.Tokaz MC, Baldomero H, Cowan AJ, Saber W, Greinix H, Koh MB, et al. An analysis of the worldwide utilization of hematopoietic stem cell transplantation for acute myeloid leukemia. Transplant Cell Ther. 2023; 29: 279.e1-10.
Search
News