Volume 7 (2024) Issue 1 No.3 Pages 14-24
Abstract
Patients undergoing allogeneic hematopoietic stem cell transplantation (HSCT) procedures often experience high levels of uncertainty. In this study, we developed and implemented a nursing intervention program to help patients recognize and reduce pre-transplant uncertainty. This study used a pretest-posttest single-group design without a control group. Eighteen patients undergoing HSCT participated in the intervention program―which included informational support, confirmation that the patients understood the information provided, and emotional support. Outpatients received the intervention at their initial outpatient visits after their procedure dates were determined, while inpatients received it at discharge following their procedures. The Universal Uncertainty in Illness Scale (UUIS), which consists of 26 items and six subscales, was used as the primary outcome measure. The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-
Introduction
Hematopoietic stem cell transplantation (HSCT) can effectively treat a number of hematologic diseases and malignancies, such as leukemia, malignant lymphoma, and aplastic anemia. In Japan, over 3,500 allogeneic HSCTs are performed annually, with a 100-day survival rate of approximately 90%. Moreover, bone marrow transplantation has improved over the past decade, yielding comparable results for both related and unrelated HSCT1. However, patients scheduled for transplantation often experience physical distress due to side effects and infections from complete induction therapy, psychological and social distress including emotional responses regarding undergoing the procedure, financial anxiety, and decreased quality of life (QOL)2, 3. Additionally, they often face uncertainty related to their illness and its treatment, which can lead to anxiety and depression4–6. While HSCT is a curative treatment, patients scheduled to undergo HSCT frequently experience psychosocial distress leading up to the procedure. Recent studies have also found evidence of uncertainty among patients undergoing HSCT7–9.
Uncertainty, as defined in Mishel's model of perceived uncertainty in illness, refers to
A recent systematic review of illness uncertainty management interventions for patients with cancer and their families found that informational support was the usual approach, provided both in-person and via telephone, along with emotional, appraisal, and instrumental support12. While gathering information is helpful in the early stages of the disease, obtaining and interpreting accurate information can be challenging. Therefore, it is important to provide accurate information on HSCT and ensure that patients fully understand the information, to help them cope with pre-treatment uncertainty13.
Nursing interventions should start before hospitalization for HSCT, to help patients recognize and reduce their uncertainties associated with the procedure7, 14. In recent years, most nursing intervention studies have focused on post-HSCT follow-up; however, to the best of our knowledge, there have been no reports in the literature on nursing intervention studies specifically targeting pre-HSCT patients to help them cope with uncertainties before undergoing the procedure15–17. Therefore, this study aimed to develop and assess the effectiveness of a nursing intervention program that would help patients scheduled to undergo HSCT recognize and reduce pre-transplant uncertainty, ultimately leading to more successful procedures. The expected study outcome was that patient uncertainty would decrease post-intervention.
Methods
Study design
This study used a pretest-posttest single-group design, without a control group.
Sample size
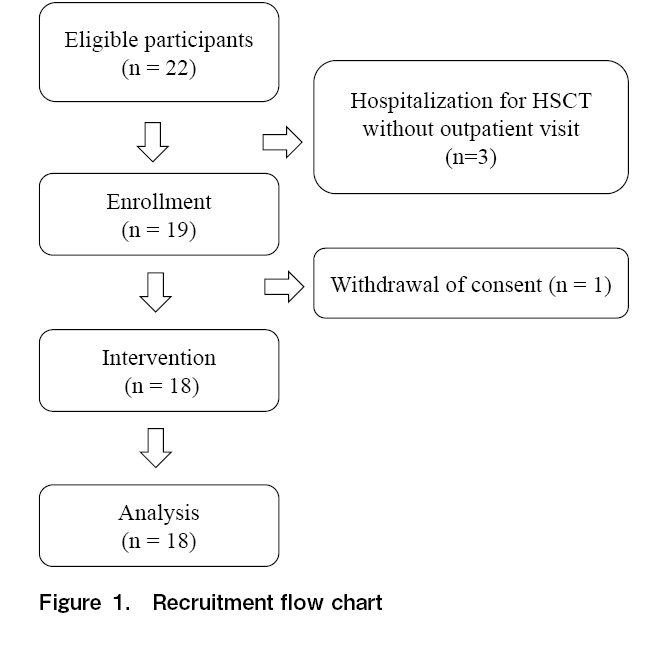
The sample size was calculated using GPower 3.1.9.7. Based on Cohen's criteria of feasibility18, the effect size was set at 0.8, the α error at 0.05, and the test power 1-β at 0.8. The necessary sample size was calculated to be 15 participants. We estimated that 25% of participants would refuse or withdraw their consent owing to physical or emotional difficulties. Therefore, we set the desired sample size at 20. Twenty-two participants enrolled in the study, but the final sample size was 18. This was because the timing of the intervention was not suitable for three patients, who were suddenly discharged from the hospital and admitted for HSCT without an outpatient visit. One other patient withdrew their consent owing to difficulty completing the study questionnaires (Figure 1).
Recruitment
This study enrolled patients who were scheduled to undergo allogeneic HSCT at Tokushima University Hospital in Japan between July 2020 and July 2022. Our inclusion criteria were as follows: patients 20 years of age or older, undergoing their first allogeneic HSCT, who had received final consent from the donor for the transplantation, and who had been given permission to participate in the study by their attending physician. The sole exclusion criterion was having a psychiatric disorder. The attending physician or hematopoietic cell transplant coordinator (HCTC) selected eligible patients and verbally explained the study's purpose to them. After obtaining verbal informed consent, each patient was referred to one of the nurses on the research team. The nurse provided a written and oral explanation of the study's purpose and obtained written informed consent from each patient.
Intervention program
Theoretical framework for Pre-HSCT uncertainty and coping
This study developed a theoretical framework for pre-transplantation uncertainty in patients undergoing HSCT, based on Mishel's model of perceived uncertainty in an illness6. Before undergoing HSCT, patients face various uncertainties concerning factors such as the disease itself, treatment options, symptoms, treatment course, and treatment environment. Nurses delivered information concerning HSCT to patients in a manner that matched their cognitive abilities. This was done to reduce pre-transplant uncertainty and help the patients deal with the challenges that transplantation presents. The expected outcomes for the patients included improved pre-HSCT QOL and reduced levels of anxiety and depression.
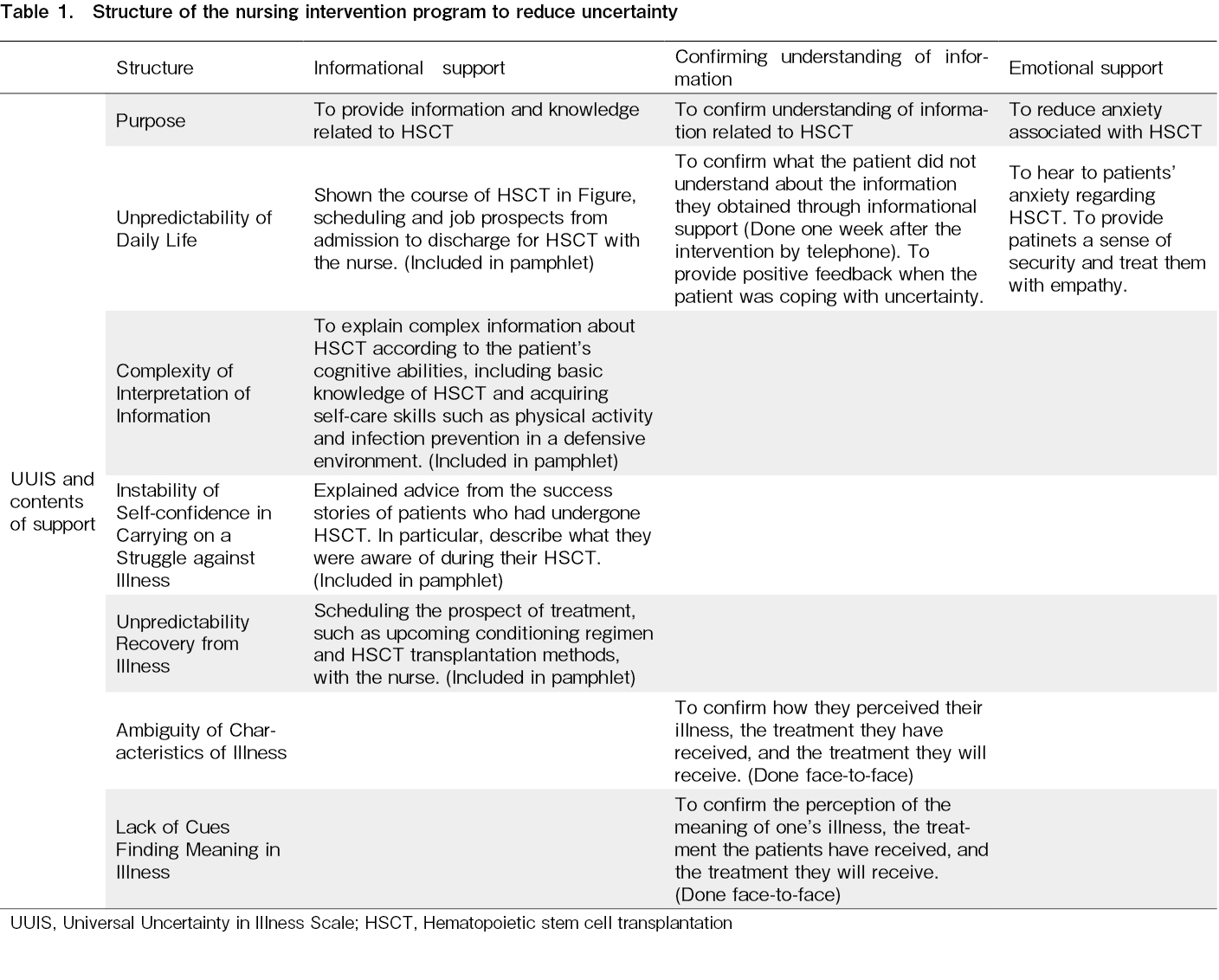
Structure and content of the program
The Universal Uncertainty in Illness Scale (UUIS), developed by Nogawa19 and based on Mishel's theory, was used in the nursing intervention program to help patients who were scheduled for HSCT reduce their levels of uncertainty. Pre-HSCT uncertainty was defined using the definitions of the UUIS subscales, and nursing intervention methods were established after reviewing relevant literature19, 20. Reinforcing knowledge with information has been proven to be effective in reducing uncertainty, and emotional support also helps promote psychosocial adjustment21. Thus, the nursing intervention program in this study: 1) provided informational support, 2) obtained confirmation of each patient's understanding of the information provided, and 3) provided emotional support (Table 1).
Informational support was provided via a pamphlet developed specifically for this study. The pamphlet contained information regarding HSCT, and the nurses used it to explain complex information to the patients based on each one's cognitive abilities20. It included basic knowledge regarding HSCT, advice on acquiring skills for physical activity and infection prevention in a defensive environment, success stories of other patients who had undergone the procedure, and recommendations regarding books and internet-based resources on HSCT. The nurses also discussed each patient's schedule from admission to discharge with the patient themselves, as well as prospective treatment schedules, upcoming conditioning regimens, and the HSCT transplantation methods their procedures would use. Each patient's HSCT progress was planned individually using an illustration provided in the pamphlet. Confirmation of each patient's understanding of the information helped to identify any aspects that were not understood. The nurses provided positive feedback to the patients to help reduce their uncertainty. The process also revealed how patients understood their illnesses and treatments as explained by their physicians, and their perceptions of their illnesses and treatment options2. As HSCT involves psychological distress, the intervention provided both informational and psychological support. Emotional support was provided to alleviate the anxiety associated with HSCT and provide a sense of security.
Content Validity of the Intervention
The intervention program was validated by a certified HSCT physician, an HCTC, and two nursing researchers. The validity of the pamphlet was confirmed by a certified HSCT physician and an HCTC. Finally, the pamphlet's content was reviewed by an HSCT survivor and the language was modified to enhance clarity.
Implementation of the Intervention
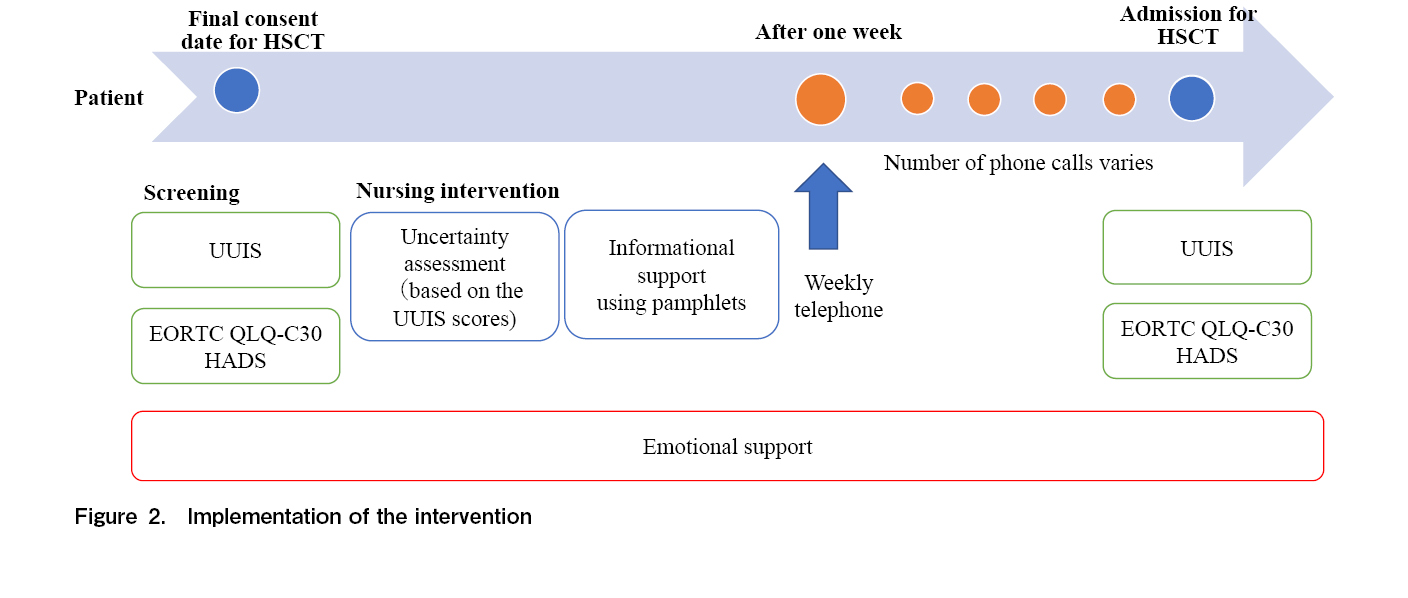
Please refer to Figure 2 for a full visual overview of how the intervention was implemented.
Uncertainty assessment (Pre-Intervention)
First, patients filled out the UUIS. Then, a nurse with a minimum of five years of experience in a hematology ward and an in-depth understanding of nursing patients with cancer conducted an uncertainty assessment. The assessment used the data collected from the UUIS questionnaire, and the patients were queried regarding the factors that contributed to their high scores if they scored 4 or 5.
Practical intervention methods
The nurse administering the UUIS explained it to the patient using pamphlets for approximately an hour, to provide information regarding HSCT. The nurse then confirmed the patient's understanding of their disease, the treatment they received, and the type of HSCT they were scheduled to undergo―as well as their perceptions of the disease and the significance of HSCT. One week later, the nurse called the patient to check if there were any aspects of HSCT that they still did not understand. The nurse also inquired about the patient's ability to address uncertainty, and provided positive feedback. Each patient received at least one support call by telephone from the same nurse. Thereafter, calls were made once per week, depending on each patient, until their admission to the hospital for their HSCT procedure. The number of phone calls varied for each patient.
Timing of the intervention
The intervention was conducted with outpatients and inpatients at different time points. Outpatients received the intervention during their earliest outpatient visit after their HSCT date was set, while inpatients received the intervention upon discharge after their HSCT date was set.
Data collection
Patient demographics
Data regarding the age, sex, disease, transplantation method, employment, and family structure of each patient were collected from their medical records.
Measures
The impact of the intervention was measured using the UUIS, European Organization for Research and Treatment of Cancer QOL Questionnaire (EORTC QLQ-C30), and the Hospital Anxiety and Depression Scale (HADS).
Universal uncertainty in illness scale
The UUIS consists of 26 items and six subscales: the unpredictability of daily life, the complexity of interpreting information, lack of cues to find meaning in the illness, ambiguous characteristics of the illness, unpredictability regarding recovery from the illness, and lack of self-confidence in carrying on the struggle against the illness19. The alpha confidence coefficient for the scale was 0.94. Scoring was based on a 5-point Likert-type scale, with higher levels of uncertainty leading to higher scores. The UUIS does not have a specific cutoff value. This study compared patient scores before and after the intervention, and a decrease in UUIS score was considered to be associated with a decrease in uncertainty.
The european organization for research and treatment of cancer QOL questionnaire
The EORTC QLQ-C30 was developed by Aaronson, and has been tested for both reliability and validity22. It consists of 30 items, including five functional scales (physical, role, social, emotional, and cognitive functioning), three symptom scales (fatigue, pain, and nausea/vomiting), six single-item scales (dyspnea, appetite loss, sleep disturbance, constipation, diarrhea, and financial impact), and a global health status scale. The scores on all scales and single-item measures range from 0-100. Higher scores on the global QOL and functioning scales indicate better health and functioning. Higher scores on the symptom and single-item scales indicate a poorer health status.
Hospital anxiety and depression scale
The HADS was developed by Zigmond23, and it was translated into Japanese by Kugaya. It consists of 14 items: seven anxiety items (HADS-A) and seven depression items (HADS-D). The Cronbach's alpha coefficient was 0.77 for the anxiety scale and 0.79 for the depression scale. Each item is rated on a 4-point Likert-type scale ranging from 0-3. Anxiety or depression scores range from 0-21 (0-7: none; 8-10: doubtful; 11-21: definite). Higher scores indicate more severe anxiety or depression.
Statistical analysis
Patient demographics were analyzed using descriptive statistics. For the UUIS and HADS, paired Student's t-tests were performed after confirming the normality of data distribution in pre- and post-tests. The EORTC QLQ-C30 was scored according to the EORTC Scoring Manual, and a Wilcoxon signed-rank sum test was performed. All statistical tests were two-tailed, and the level of statistical significance was set at p = 0.05. Statistical analyses were performed using SPSS version 29.0 (Armonk, NY, US).
Ethical approval
The study protocol was approved by the ethics committee of Tokushima University Hospital (approval no. 3757), and the study was performed in accordance with the latest version of the Helsinki Declaration. The intervention was conducted after enrollment of the study in the UMIN Clinical Trials Registry (UMIN000040421). All patients received informational pamphlets and provided written informed consent before the intervention. To protect patient privacy, all interventions were conducted in private rooms.
Results
Patient demographics
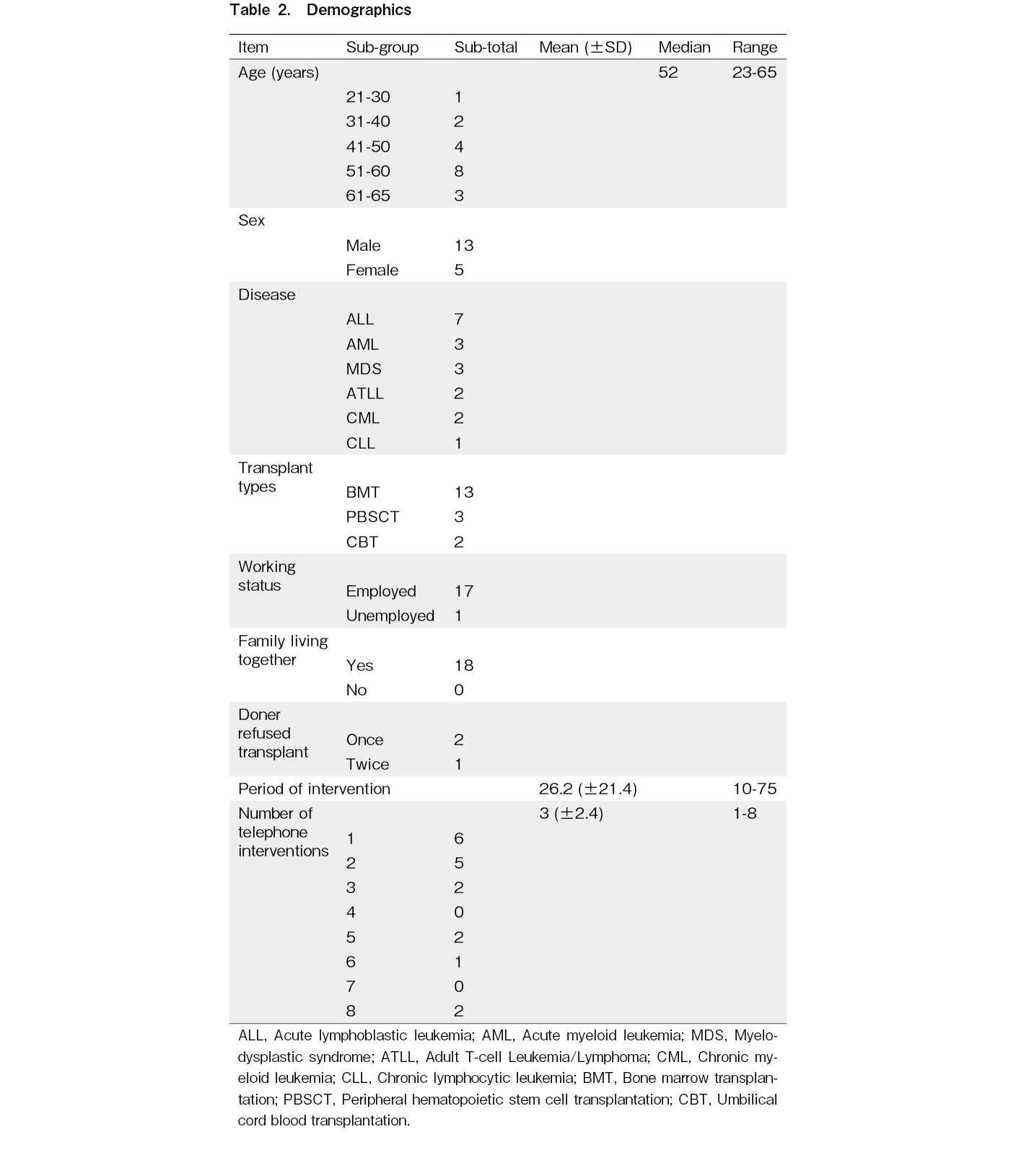
Eighteen patients (13 male and five female participants) with a median age of 52 years participated in the study. All of the patients were undergoing HSCT for the first time. Seven patients had acute lymphoblastic leukemia, and 13 were scheduled for bone marrow transplantations. Most of the patients were employed, and all had family members living with them. Three of the patients were refused a transplant from their first or second donor. The average number of intervention days was 26 (range, 10-75) days, the average number of telephone interventions was three (range, 1-8), and the average duration of each telephone call was 19.78 min (Table 2).
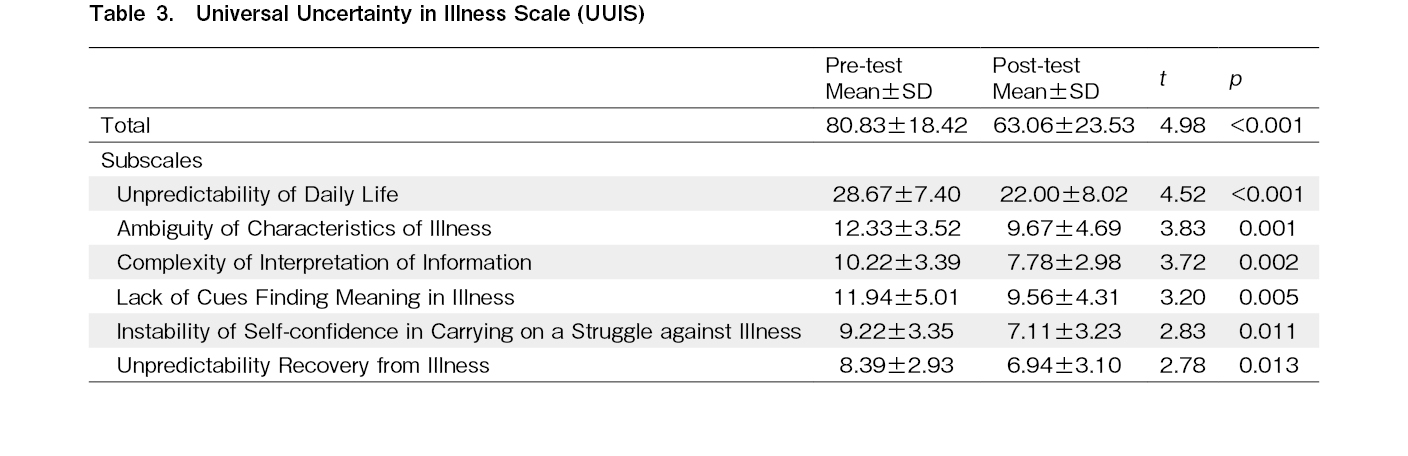
The UUIS
The total UUIS score decreased significantly, from 80.83 ± 18.42 pre-intervention to 63.06 ± 23.53 post-intervention (t = 4.98, p < 0.001). All six subscales of the UUIS also decreased significantly post-intervention: unpredictability of daily life decreased from 28.67 ± 7.40 pre-intervention to 22.00 ± 8.02 post-intervention (t = 4.52, p < 0.001); ambiguous characteristics of the illness decreased from 12.33 ± 3.52 pre-intervention to 9.67 ± 4.69 post-intervention (t = 3.83, p = 0.001); and complexity of interpreting information decreased from 10.22 ± 3.39 pre-intervention to 7.78 ± 2.98 post-intervention (t = 3.72, p = 0.002; Table 3).
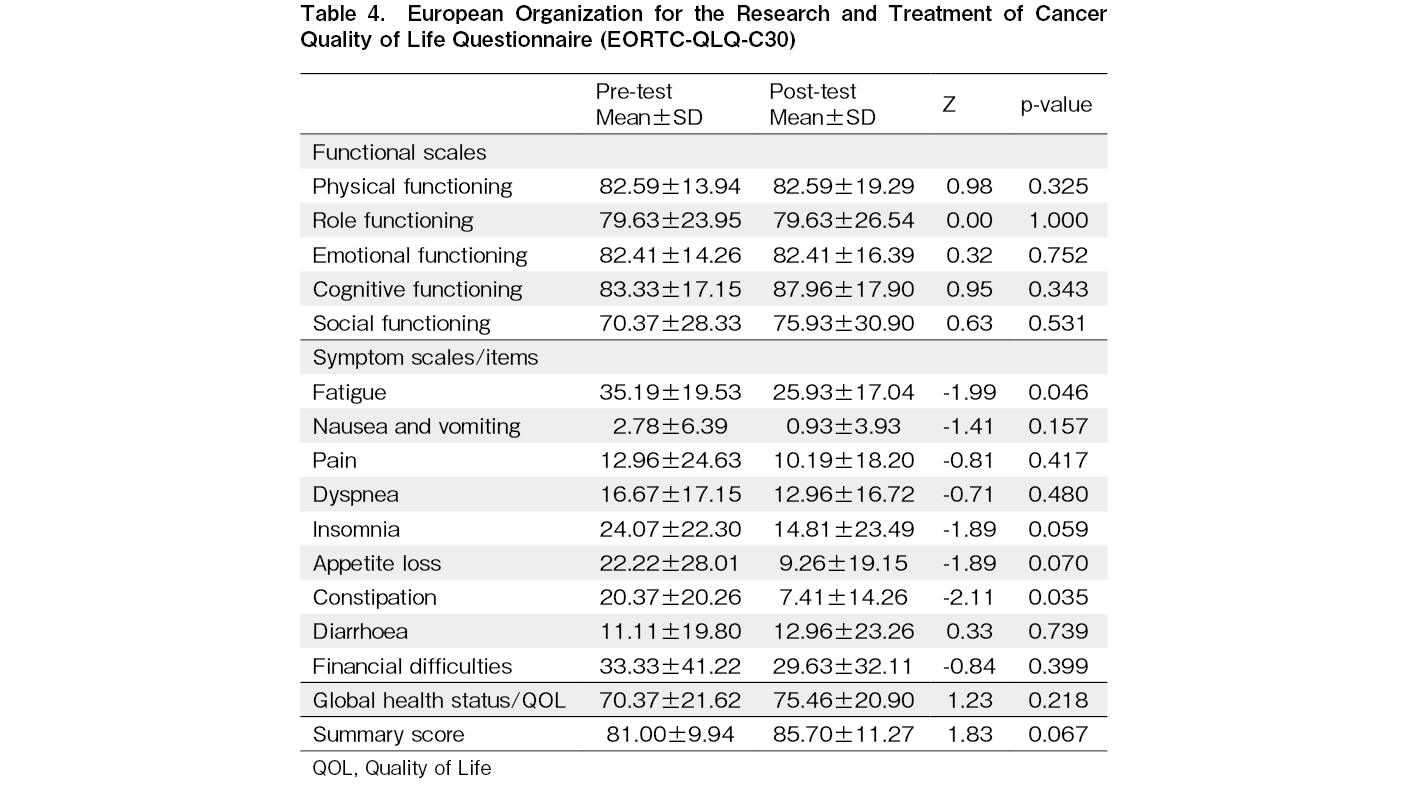
The EORTC QLQ-C30
The functional EORTC QLQ-C30 scale scores did not differ significantly. The symptom scale showed a significant decrease in fatigue (pre = 35.19 ± 19.53, post = 25.93 ± 17.04, Z = -1.99, p < 0.046) and constipation (pre = 20.37 ± 20.26, post = 7.41 ± 14.26, Z = -2.11, p = 0.035), but no significant differences in the other symptoms. Similarly, global health status/QOL did not differ significantly (Table 4).
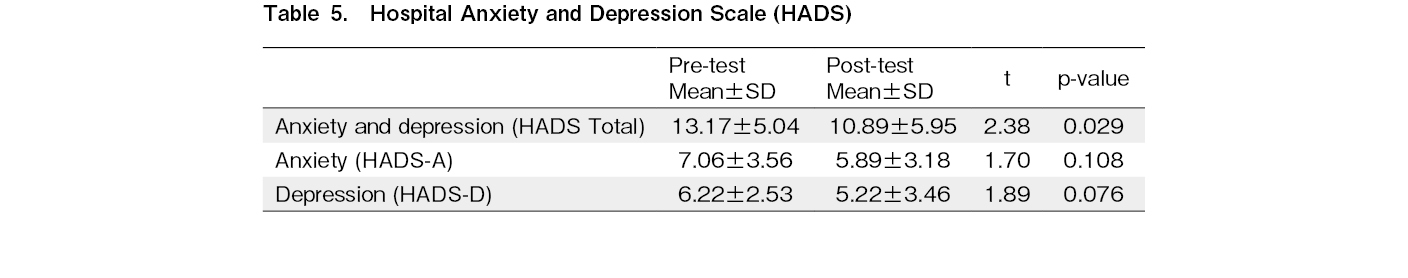
The HADS
The total HADS score decreased significantly, from 13.17 ± 5.04 pre-intervention to 10.89 ± 5.95 post-intervention (t = 2.38, p = 0.029); however, there was no significant difference in anxiety (pre = 7.06 ± 3.56, post = 5.89 ± 3.18, t = 1.70, p = 0.108). There was no significant difference in depression as well (pre = 6.22 ± 2.53, post = 5.22 ± 3.46, t = 1.89, p = 0.076). None of the patients scored more than 11 points in terms of anxiety or depression (Table 5).
Discussion
The results showed that the UUIS scores decreased significantly post-intervention compared to pre-intervention. The effects of providing informational support and confirmation that the patients understood the information presented to them are discussed below.
Effects of providing informational support
During informational support, patients were provided with information regarding HSCT based on their cognitive abilities, through pamphlets. This resulted in decreases in four subscales: unpredictability of daily life, complexity of interpretation of information, lack of self-confidence in carrying on the struggle against the illness, and unpredictability of recovery from the illness.
Unpredictability of daily life refers to patients not knowing whether they will be able to continue their usual routines and roles following HSCT19. This uncertainty was addressed by providing each patient with a pamphlet containing a diagram that explained the HSCT process. The pamphlet also mentioned what to expect throughout the treatment process, starting from the date of admission to discharge. It is important for patients to understand how their treatment will affect their daily lives and work before undergoing HSCT, so this type of information can help them better focus on the transplantation.
The complexity of interpreting the information refers to the uncertainty that patients experience when they lack the necessary information about the disease or HSCT19. To address this uncertainty, pamphlets were provided and nurses explained the basics of HSCT and the skills needed, in a safe environment. Providing information is a key strategy for managing uncertainty in patients24, but it is also important to help patients meet their informational needs using other sources. Nurses involved with patients can use books and online resources to provide information, solve problems, and offer their patients additional options when they lack information.
Lack of self-confidence in carrying on the struggle against the illness refers to a patient not knowing whether their body will react positively to HSCT19. Before treatment, patients experience emotional fluctuations regarding whether they should undergo HSCT. This is because they realize that HSCT is a highly invasive treatment that may result in prolonged hospitalization, and they are uncertain of their chances of survival2. It is important for them to learn from patients who have undergone HSCT, to help them achieve a positive perspective on the procedure. For this purpose, we created a pamphlet to explain interventions for this type of uncertainty, which included advice from patients who had successfully undergone HSCT. The purpose of the pamphlet was to assist the patients in this study with viewing HSCT as a necessary step in curing their diseases.
Unpredictability of recovery from the illness refers to a patient being uncertain about the possible outcomes of their disease, such as not being in complete remission or relapsing before undergoing HSCT4, 20. To address this form of uncertainty, prospective treatment schedules were arranged between each patient and their nurse. This included upcoming conditioning regimens and transplantation methods. Even when it is difficult to predict the future, having a detailed treatment plan for a patient's return to normal life before their admission to undergo HSCT can help them get through the procedure without losing hope25.
Effect of confirmoffing that patients understood the presented information
Confirming that the patients understood the information they were provided allowed us to identify which aspects of informational support they struggled to comprehend. In addition to providing accurate information using the pamphlet, the nurses also verified whether the patients understood the information, and if they did not understand something the nurses helped explain it, thereby reducing uncertainty preceding HSCT. Confirming each patient's perception of their disease and treatment options via explanations from their doctors can reduce ambiguity surrounding the illness and the lack of clarity surrounding the meanings of illness subscales.
Ambiguous characteristics of the illness refers to patient uncertainties surrounding their illnesses and the prior treatments received19. Patients often have an ambiguous understanding of their disease and treatment because the content, amount, and timing of information are not provided in a setting that is appropriate to each patient's ability to understand26. In our study, this uncertainty was addressed by identifying how our patients perceived their diseases, the treatments they had previously received, and the treatment that they would receive. For patients who were unable to explain the progress of their disease or treatment, the nurse supplemented explanations with medical records. It is crucial to evaluate how well patients comprehend their diseases and treatments, in order to understand the treatment aspects of HSCT.
Lack of cues to find meaning in the illness refers to the uncertainty of not knowing the meaning of one's disease or treatment19. This uncertainty was addressed by confirming each patient's perception of the meaning of their illness, the treatments they received previously, and the treatment that they would receive. Meaning-making regarding diseases and HSCT has been reported to enhance positive personal growth and adaptive coping27. Patients should recognize what it means to undergo HSCT, to enable them to prepare for a long and painful treatment process.
Effect on QOL and the HADS
In this study, reducing uncertainty was predicted to be helpful for improving QOL and decreasing depression and anxiety; however, there were no changes in these indicators following the intervention. Compared to previous studies that applied the EORTC QLQ-C30 prior to HSCT procedures, the patients in this study scored better on the functional and symptom scale items, suggesting no change resulting from the intervention28. Fatigue was reported to be highest during treatment and improved preceding HSCT, after a certain amount of time had elapsed since chemotherapy was last administered. Similarly, constipation also improved in most patients as their HSCT procedures approached, which aligns with findings from previous studies29.
Although reported to be high preceding HSCT30, our intervention did not seem to affect patient anxiety. It has been reported that approximately 30% of patients are depressed before HSCT31. However, in the present study, none of the patients were found to be depressed before HSCT; therefore, there was no change in depression following our intervention. Depression is a factor that impacts QOL; therefore, the prevention of depression is important to improving QOL14. It is also important to assess QOL and depression before HSCT, because low levels of problem-solving have been reported to increase depression and decrease QOL32.
Implications for nursing
It is important to assess uncertainty before patients undergo HSCT, so they can better prepare themselves. Nurses can not only provide information to their patients, but also supplement and provide information based on each patient's cognitive status. This helps to resolve the complexity surrounding understanding the disease and its treatment. Useful ways of helping patients deal with uncertainty include confirming their understanding of the information, addressing questions together if they do not understand something, and teaching problem-solving strategies. It is necessary for patients to understand their diseases and treatment options, as well as perceive them in a positive manner, to help cure said diseases and facilitate earlier adaptation to HSCT33.
Limitations
This was a pre-and-post study conducted at a single institution. The number of calls varied depending on each patient's situation (e.g., early admission due to COVID-19, or HSCT donor changes), which affected the results. Moreover, it was not possible to determine whether the patients were able to successfully address their uncertainties; therefore, our results should be interpreted with some caution. Future studies should identify the factors that influence perceptions of uncertainty in a larger cohort, thereby providing a more efficient intervention for patients with low understanding.
Conclusion
This study examined the effectiveness of a nursing intervention program aimed at reducing patient uncertainty leading up to HSCT. It proved to be successful in reducing all of the UUIS total and subscale scores for pre-HSCT uncertainties.
Acknowledgments
The authors thank all the patients who participated in this study. We also thank Dr. Hirokazu Miki and Dr. Takeshi Harada of the Department of Hematology, Endocrinology, and Metabolism, Tokushima University Graduate School of Biomedical Sciences; Dr. Hiroyoshi Watanabe of the Department of Pediatrics, Tokushima University Graduate School of Biomedical Sciences; nurses at the Cell Therapy Center, Tokushima University Hospital; and nurses at the Internal Medicine Outpatient Clinic. Finally, we are grateful to Ms. Takako Otani of the Japan Marrow Donor Program and Ms.
Author Contributions
K.N., S.Y., and A.H designed the study. K.N., S.F., A.F., and K. K. screened the patients. S.F obtained informed consent. K.N. collected the data. K.N. and Y.A. analyzed the data. K.N., S.F., A.F., K.K., Y.A., M.A.,
Conflicts of Interest
The authors declare no conflict of interest. Disclosure forms provided by the authors are available on the website.
Acknowledgments
The authors thank all the patients who participated in this study. We also thank Dr. Hirokazu Miki and Dr. Takeshi Harada of the Department of Hematology, Endocrinology, and Metabolism, Tokushima University Graduate School of Biomedical Sciences; Dr. Hiroyoshi Watanabe of the Department of Pediatrics, Tokushima University Graduate School of Biomedical Sciences; nurses at the Cell Therapy Center, Tokushima University Hospital; and nurses at the Internal Medicine Outpatient Clinic. Finally, we are grateful to Ms. Takako Otani of the Japan Marrow Donor Program and Ms.
Funding Statement
This study was supported by the Foundation for the Promotion of Cancer Research in Japan (in 2021).
Acknowledgments
The authors thank all the patients who participated in this study. We also thank Dr. Hirokazu Miki and Dr. Takeshi Harada of the Department of Hematology, Endocrinology, and Metabolism, Tokushima University Graduate School of Biomedical Sciences; Dr. Hiroyoshi Watanabe of the Department of Pediatrics, Tokushima University Graduate School of Biomedical Sciences; nurses at the Cell Therapy Center, Tokushima University Hospital; and nurses at the Internal Medicine Outpatient Clinic. Finally, we are grateful to Ms. Takako Otani of the Japan Marrow Donor Program and Ms.
Ethics Approval
The study protocol was approved by the ethics committee of Tokushima University Hospital (No. 3757) and was performed in accordance with the latest version of the Helsinki Declaration.
Acknowledgments
The authors thank all the patients who participated in this study. We also thank Dr. Hirokazu Miki and Dr. Takeshi Harada of the Department of Hematology, Endocrinology, and Metabolism, Tokushima University Graduate School of Biomedical Sciences; Dr. Hiroyoshi Watanabe of the Department of Pediatrics, Tokushima University Graduate School of Biomedical Sciences; nurses at the Cell Therapy Center, Tokushima University Hospital; and nurses at the Internal Medicine Outpatient Clinic. Finally, we are grateful to Ms. Takako Otani of the Japan Marrow Donor Program and Ms.
Informed Consent
Eighteen patients received the information pamphlets and provided written informed consent before starting the intervention.
Acknowledgments
The authors thank all the patients who participated in this study. We also thank Dr. Hirokazu Miki and Dr. Takeshi Harada of the Department of Hematology, Endocrinology, and Metabolism, Tokushima University Graduate School of Biomedical Sciences; Dr. Hiroyoshi Watanabe of the Department of Pediatrics, Tokushima University Graduate School of Biomedical Sciences; nurses at the Cell Therapy Center, Tokushima University Hospital; and nurses at the Internal Medicine Outpatient Clinic. Finally, we are grateful to Ms. Takako Otani of the Japan Marrow Donor Program and Ms.
Clinical Trial Number and Registry URL
The intervention was initiated after enrollment in the UMIN Clinical Trials Registry (UMIN000040421).
URL: https://center6.umin.ac.jp/cgi-open-bin/ctr/ctr_view.cgi?recptno=R000046049
References
1.Japanese Data Center for Hematopoietic Cell Transplantation. Hematopoietic cell transplantation in Japan. Annual report of nationwide survey 2021. http://www.jdchct.or.jp/en/data/slide/2021/ [Accessed: 2 April 2023]
2.Mori K. Development of a nursing intervention program to support intrinsic motivation-based decision making by patients undergoing hematopoietic stem cell transplantation. J Jpn Soc Cancer Nurs. 2008; 22: 55-64.
3.Morishita S, Kaida K, Ikegame K, Yoshihara S, Taniguchi K, Okada M, et al. Impaired physiological function and health-related QOL in patients before hematopoietic stem-cell transplantation. Support Care Cancer. 2012; 20: 821-9.
4.Goetzmann L, Klaghofer R, Wagner-Huber R, Halter J, Boehler A, Muellhaupt B, et al. Quality of life and psychosocial situation before and after a lung, liver or an allogeneic bone marrow transplant – Results from a prospective study. Swiss Med Wkly. 2006; 136: 281-90.
5.Syrjala KL, Yi JC, Langer SL. Psychometric properties of the Cancer and Treatment Distress (CTXD) measure in hematopoietic cell transplantation patients. Psychooncology. 2016; 25: 529-35.
6.Mishel MH. Uncertainty in illeness. J Nurs Sch. 1988; 20: 225-32.
7.Adarve SE, Osorio JH. Factors associated with uncertainty in patients scheduled to undergo hematopoietic stem cell transplantation. Cancer Nurs. 2020; 43: E335-41.
8.Kusaka K, Inoguchi H, Nakahara R, Kurosawa S, Fukuda T, Satomura K, et al. Stress and coping strategies among allogeneic haematopoietic stem cell transplantation survivors: A qualitative study. Eur J Cancer Care (Engl). 2020; 29: e13307.
9.Kuba K, Esser P, Scherwath A, Schirmer, Schulz-Kindermann F, Dinkel A, et al. Cancer-and-treatment-specific distress and its impact on posttraumatic stress in patients undergoing allogeneic hematopoietic stem cell transplantation (HSCT). Psychooncology. 2017; 26: 1164-71.
10.Mishel MH. Perceived uncertainty and stress in illness. Res Nurs Health. 1984; 7: 163-71.
11.Farsi Z, Nayeri ND, Negarandeh R. The coping process in adults with acute leukemia undergoing hematopoietic stem cell transplantation. J Nurs Res. 2012; 20: 99-109.
12.Guan T, Qan'ir Y, Song LX. Systematic review of illness uncertainty management interventions for cancer patients and their family caregivers. Support Care Cancer. 2021; 29: 4623-40.
13.Farsi Z, Nayeri ND, Negarandeh R. Coping strategies of adults with leukemia undergoing hematopoietic stem cell transplantation in Iran: A qualitative study. Nurs Health Sci. 2010; 12: 485-92.
14.Song CE, So HS. Factors influencing changes in quality of life in patients undergoing hematopoietic stem cell transplantation: A longitudinal and multilevel analysis. J Korean Acad Nurs. 2015; 45: 694-703.
15.White LL, Kupzyk KA, Berger AM, Cohen MZ, Bierman PJ. Self-efficacy for symptom management in the acute phase of hematopoietic stem cell transplant: A pilot study. Eur J Oncol Nurs. 2019; 42: 21-7.
16.van der Lans MCM, Oldenmenger WH, van der Stege HA, van Staa A, Molendijk A, Broers AEC. Evaluation of a nurse-led patient navigation intervention follow-up of patients after autologous and allogeneic stem cell transplantation. Cancer Nurs. 2022; 45: 287-96.
17.Schmidt H, Boese S, Bauer A, Landenberger M, Lau A, Stoll O, et al. Interdisciplinary care programme to improve self-management for cancer patients undergoing stem cell transplantation: A prospective non-randomised intervention study. Eur J Cancer Care. 2017; 26.
18.Cohen J. Chapter 1. In: Statistical Power Analysis for the Behavioral Sciences, 2nd ed., Hillsdale, Erlbaum. 1988; 19-35.
19.Nogawa M. Development of a Universal Uncertainty in Illness Scale to be used for inpatients and outpatients. J Jpn Acad Nurs Sci. 2012; 32: 3-11.
20.Mishel MH, Germino BB, Lin L, Pruthi RS, Wallen EM, Crandell J, et al. Managing uncertainty about treatment decision making in early stage prostate cancer: A randomized clinical trial. Patient Educ Couns. 2009; 77: 349-59.
21.Gumus AB, Cam O. Effects of emotional support-focused nursing interventions on the psychosocial adjustment of breast cancer patients. Asian Pac J Cancer Prev. 2008; 9: 691-7.
22.Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez N, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993; 85: 365-76.
23.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983; 67: 361-70.
24.Mishel MH, Belyea M, Germino BB, Stewart JL, Bailey DE Jr, Robertson C, et al. Helping patients with localized prostate carcinoma manage uncertainty and treatment side effects – Nurse-delivered psychoeducational intervention over the telephone. Cancer. 2002; 94: 1854-66.
25.Farsi Z, Nayeri ND, Negarandeh R. The coping process in adults with acute leukemia undergoing hematopoietic stem cell transplantation. Nurs Res. 2012; 20: 99-109.
26.Mishel MH, Germino BB, Belyea M, Stewart JL, Bailey DE Jr, Mohler J, et al. Moderators of an uncertainty management intervention: for men with localized prostate cancer. Nurs Res. 2003; 52: 89-97.
27.Adelstein KE, Anderson JG, Taylor AG. Importance of meaning-making for patients undergoing hematopoietic stem cell transplantation. Oncol Nurs Forum. 2014; 41: E172-84.
28.Grulke N, Albani C, Bailer H. Quality of life in patients before and after haematopoietic stem cell transplantation measured with the European Organization for Research and Treatment of Cancer (EORTC) Quality of Life Core Questionnaire QLQ-C30. Bone Marrow Transplant. 2012; 47: 473-82.
29.Larsen J, Nordström G, Björkstrand B, Ljungman P, Gardulf A. Symptom distress, functional status and health-related quality of life before high-dose chemotherapy with stem-cell transplantation. Eur J Cancer Care. 2003; 12: 71-80.
30.Seo HJ, Baek YG, Cho BS, Kim TS, Um YH, Chae JH. Anxiety and depression of the patients with hematological malignancies during hospitalization for hematopoietic stem cell transplantation. Psychiatry Investig. 2019; 16: 751-8.
31.Kettmann JDJ, Altmaier EM. Social support and depression among bone marrow transplant patients. J Health Psychol. 2008; 13: 39-46.
32.Nezu AM, Nezu CM, Houts PS, Friedman SH, Faddis S. Relevance of problem-solving therapy to psychosocial oncology. J Psychosocial Oncol. 1999; 16: 5-26.
33.Baliousis M, Rennoldson M, Dawson DL, Mills J, das Nair R. Perceptions of hematopoietic stem cell transplantation and coping predict emotional distress during the acute phase after transplantation. Oncol Nurs Forum. 2017; 44: 96-107.
Search
News