Volume 5 (2022) Issue 3 No.4 Pages 83-86
Abstract
Introduction: There are existing international guidelines for long-term follow-up (LTFU) care of allogeneic hematopoietic cell transplantation (allo-HCT) survivors. However, implementing these guidelines represents a unique challenge in resource-challenged settings.
Methods: This study aimed to evaluate adherence to recommended surveillance in allo-HCT survivors at an academic center in North India and study the incidence of late effects. This single-center, retrospective study analyzed records of allo-HCT recipients from 2016 to 2020. Survivors were screened in our LTFU clinic at day +100 and +365 using cardiometabolic parameters (screening for hypertension, dyslipidemia, hyperglycemia, 24-hour urine protein, thyroid function), pulmonary function test (PFT), bone mineral density (BMD), and initiation of revaccination.
Results: A total of 40/80 (50%) allo-HCT survivors were alive at a median of 888 days (IQR 515-1,306). The adherence to home-based screening parameters such as blood pressure and blood glucose was highest (
Conclusion: The adherence to recommended surveillance measures for allo-HCT survivors in an academic LTFU clinic at one year was only 75% overall. Cardiometabolic abnormalities were noted in more than half of the survivors. This study emphasizes the need for a structured LTFU clinic in all centers performing HCT.
Introduction
It is well known that the life expectancy of allo-HCT survivors is lower than the general population due to several late side effects1. There are international consensus guidelines for recommended screening and preventive practices for LTFU care of HCT survivors2. However, adherence to these guidelines in
Methods
Our center is a 10-bed HCT center performing 50-60 autologous+allo-HCT since 2008. The LTFU clinic was started in 2016 and is run weekly by a team of faculty members, senior residents, and medical social workers in liaison with other specialists when needed. Allo-HCT survivors are evaluated in our LTFU clinic at day +100 and +365 and annually thereafter for late effects according to international guidelines2. The institutional ethics committee cleared the study. The medical records up to one-year post-HCT of all consecutive patients who underwent allo-HCT from April 2016 to December 2020 were analyzed. The parameters analyzed were cardiometabolic surveillance (screening for hypertension, dyslipidemia, hyperglycemia, 24-hour urine protein examination, thyroid function), pulmonary function test (PFT), bone mineral density (BMD) by dual-energy X-ray absorptiometry (DXA) scan, and initiation of revaccination. As most patients in our cohort were pre-menopausal women and men <50-years, Z-score
Results
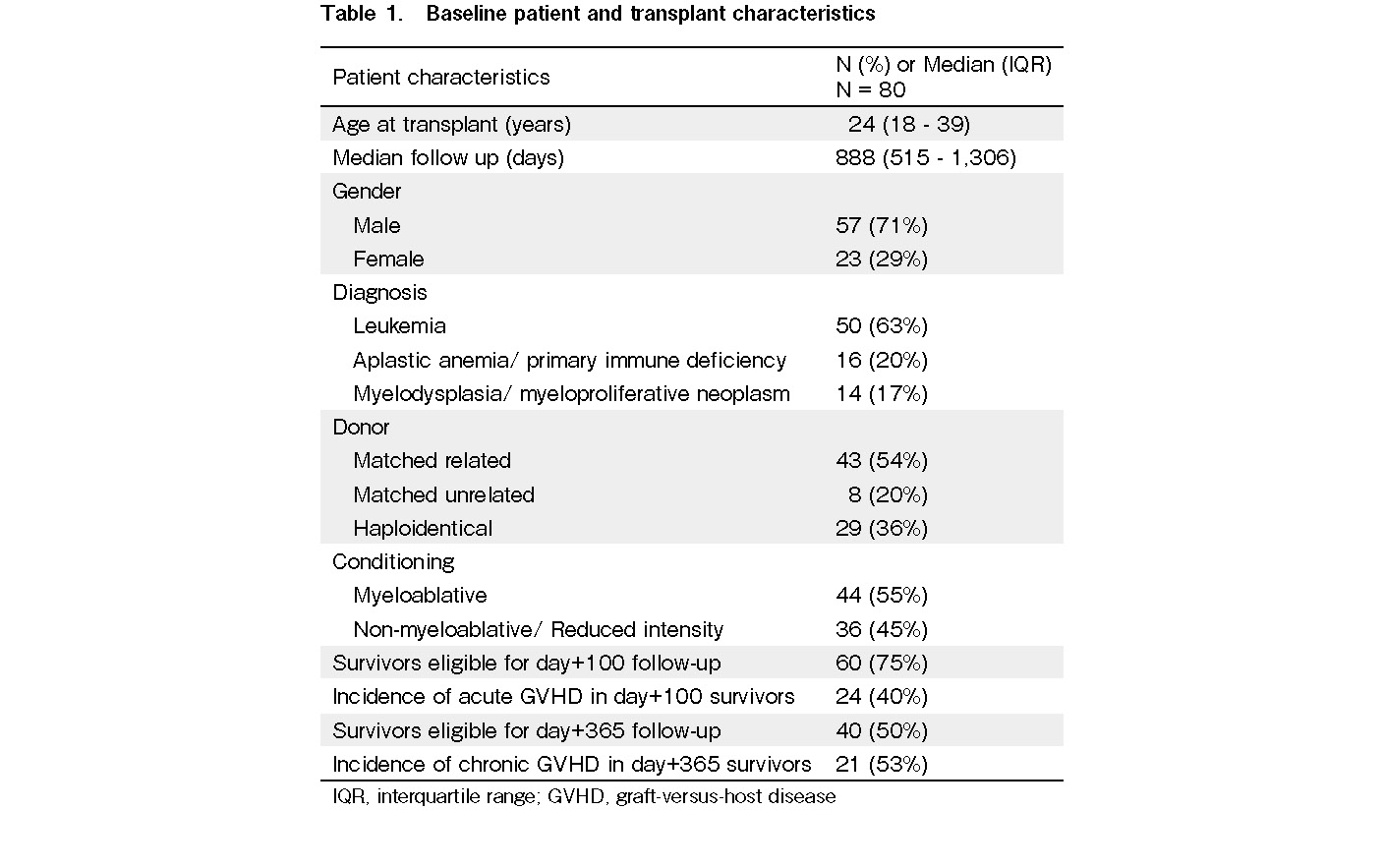
Of the 80 patients who underwent allo-HCT at our center during the study period, 60 and 40 survivors were eligible for the day +100 and +365 follow-up, respectively (Table 1). The median follow-up duration of the survivors was 888 days (IQR: 515-1,306 days). No patients were lost to follow-up in our cohort. The cohort's median age was 24 years (IQR, 18-39 years), and there was a male preponderance (n=57, 71%). The most common indication for transplantation was leukemia (n=50, 63%), followed by aplastic anemia/primary immunodeficiency (n=16, 20%), and myelodysplasia/
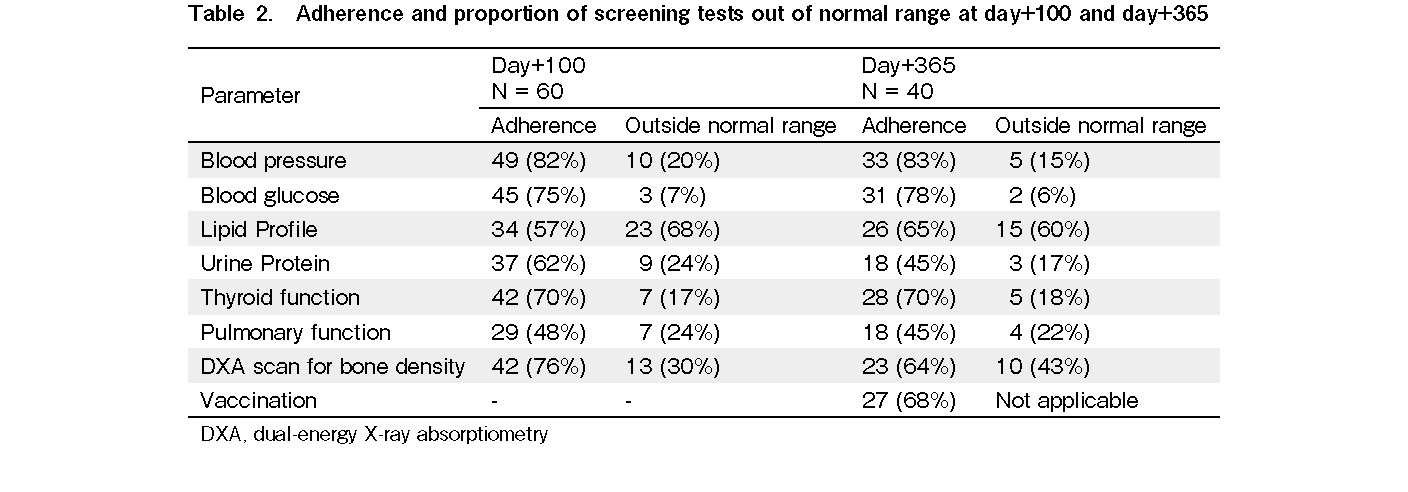
Adherence to home-based screening parameters, including blood pressure and blood glucose, was >75% at both day +100 and +365 (Table 2). The adherence to other lab-based cardiometabolic screening parameters varied from 45% to 70% at each time point. The adherence to specialized lab-based tests, such as PFT, was the lowest at under 50% at either time point. The adherence to the DXA scan for bone density was relatively high (76% at day +100 and 64% at day +365). Adherence to the initiation of revaccination on day
Discussion
Data regarding adherence to LTFU care of allo-HCT survivors are scarce in the literature, specifically from resource-challenged regions. In a recent American Society for Blood and Marrow Transplantation (ASBMT) online survey of transplant centers in North America, only 45% had a dedicated LTFU clinic. Lack of expertise, logistics, financial issues, and practitioners' preference to provide survivorship care are obstacles to establishing new LTFU clinics7. The median adherence to LTFU survivorship care recommendations in resource-rich settings beyond two years post-HCT was 75%8. This study identified autologous transplant, concerns about costs, non-white race, male sex, lower physical functioning status, absence of chronic GVHD, longer time since transplant, and lack of knowledge regarding the recommended tests as factors associated with poor adherence. In a recent study from Japan, only 5.8% failed screening in an automatically ordered electronic health record system. The reasons cited were equally distributed between no patient consent, physician decision, or forgot to order9. There are no data on how many transplant programs in India or resource-challenged settings have LTFU clinics. Being in an academic center at an institute of national importance, we had the resources and motivation to run a structured LTFU clinic for the past five years. Despite this, the overall adherence to LTFU survivorship care at one year was 75%. Adherence in centers without LTFU clinics in the rest of the country could be even lower. Although the factors for nonadherence were not addressed in this short-term follow-up study, poor health literacy may be one of the reasons. The fact that adherence to home-based screening was the highest, followed by lab-based and specialized tests, shows that this could also be due to ease of access. The concurrent implementation of a prospective study and clinical trial in our department (CTRI/2019/04/018764) accounts for the high adherence to BMD monitoring10. The current data show that at least 80% of the study population could benefit from the monitoring schedule because at least one actionable out-of-range parameter could be identified. Although our patient numbers were small and the follow-up was short to demonstrate any effect on morbidity and mortality, several extensive studies have established a relationship between cardiovascular events in HCT survivors with metabolic syndrome11. The Indian population is also otherwise at a higher risk of cardio-metabolic and bone health complications than other ethnicities12,13. The data from this study may not reflect other centers across the region without established LTFU clinics and survivorship care protocols. Overall, the current study reinforces the need to establish a systematic LTFU clinic and protocol in transplant centers, even in resource-challenged settings. A patient-centered approach using a personalized survivorship care plan (SCP) and digital health can improve adherence to recommended surveillance measures in India (CTRI/2021/08/035686).
Author Contributions
NSK, AJ, NSM, PM and DPL contributed to the study conception and design. Data collection and analysis were performed by all authors. The first draft of the manuscript was written by NSK, DPL and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Financial Support
The study was partly funded by the American Society of Hematology (ASH) Global Research Award to DPL.
Ethical Approval
The study was cleared by the intuitional ethics committee of Postgraduate Institute of Medical Education and Research, Chandigarh, India, INT/IEC/2021/SPL-982.
Informed Consent
Informed consent was obtained from all participants included in the study.
Conflicts of Interest
The authors declare no conflict of interest. Disclosure forms provided by the authors are available on the website.
References
1.Martin PJ, Counts GW Jr, Appelbaum FR, Lee SJ, Sanders JE, Deeg HJ, et al. Life expectancy in patients surviving more than 5 years after hematopoietic cell transplantation. J Clin Oncol. 2010; 28: 1011-6.
2.Majhail NS, Rizzo JD, Lee SJ, Aljurf M, Atsuta Y, Bonfim C, et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation. Bone Marrow Transplant. 2012; 47: 337-41.
3.Indian Society For Blood And Marrow Transplantation (ISBMT) Registry-2020.
4.Pasquini MC, Srivastava A, Ahmed SO, Aljurf M, Atsuta Y, Doleysh C, et al. Worldwide Network for Blood and Marrow Transplantation Recommendations for Establishing a Hematopoietic Cell Transplantation Program, Part I: Minimum Requirements and Beyond. Biol Blood Marrow Transplant. 2019; 25: 2322-9.
5.John MJ, Mathew A, Bhat S, Prabhakaran A, George B, John J. Post stem cell transplantation revaccination: A survey of the current practices in India. Vaccine. 2018; 36: 2176-80.
6.International Society for Clinical Densitometry (ISCD) adult official position,
7.Hashmi SK, Lee SJ, Savani BN, Burns L, Wingard JR, Perales MA, et al. ASBMT Practice Guidelines Committee Survey on Long-Term Follow-Up Clinics for Hematopoietic Cell Transplant Survivors. Biol Blood Marrow Transplant. 2018; 24: 1119-24.
8.Khera N, Chow EJ, Leisenring WM, Syrjala KL, Baker KS, Flowers ME, et al. Factors associated with adherence to preventive care practices among hematopoietic cell transplantation survivors. Biology of blood and marrow transplantation. Biol Blood Marrow Transplant. 2011; 17: 995-1003.
9.Kurosawa S, Yamaguchi T, Mori A, Tsukagoshi M, Okuda I, Ikeda M, et al. Feasibility and usefulness of recommended screenings at long-term follow-up clinics for hematopoietic cell transplant survivors. Support Care Cancer. 2022; 30: 2767-76.
10.Khaire N DA, Sinha A, Bhadada S, Malhotra P, Khadwal A, Prakash G, et al. Early bone loss in Indian patients undergoing allogeneic hematopoietic cell transplantation. Blood Cell and Therapy. 2021; 3: 48-53.
11.Greenfield DM, Salooja N, Peczynski C, van der Werf S, Schoemans H, Hill K, et al. Metabolic syndrome and cardiovascular disease after haematopoietic cell transplantation (HCT) in adults: an EBMT cross-sectional non-
12.Volgman AS, Palaniappan LS, Aggarwal NT, Gupta M, Khandelwal A, Krishnan AV, et al. Atherosclerotic Cardiovascular Disease in South Asians in the United States: Epidemiology, Risk Factors, and Treatments: A Scientific Statement From the American Heart Association. Circulation. 2018; 138: e1-34.
13.Mithal A, Bansal B, Kyer CS, Ebeling P. The Asia-Pacific Regional Audit-Epidemiology, Costs, and Burden of Osteoporosis in India 2013: A report of International Osteoporosis Foundation. Indian J Endocrinol Metab. 2014; 18: 449-54.
Search
News