Volume 5 (2022) Issue 2 No.1 Pages 35-44
Abstract
Purpose: To examine the relationship between health-related quality of life (HRQOL) and fulfillment of informational needs among patients for allogeneic hematopoietic stem cell transplant (HSCT) and caregivers who visit long-term follow-up (LTFU) clinics within 1.5 years of post-HSCT.
Methods: We conducted a cross-sectional survey at two university hospitals in Japan between May and December 2018 using self-administered questionnaires and medical records. Based on previous research and patient interviews, informational needs of patients and caregivers were categorized into general information, post-discharge treatments, side effects and complications, self-care, psychosocial problems, and social resources. The HRQOL of patients and caregivers was measured using the Japanese Functional Assessment of Cancer Therapy-Bone Marrow Transplant (for patients) and Caregiver Quality of Life Index-Cancer (for caregivers). In addition, the pooled-regression actor-partner interdependence model approach was employed to analyze the relationships using R ver.3.6.0.
Results: A total of 16 patients and 14 caregivers were analyzed. The mean total score of the FACT-BMT was 91.0, and the mean total score of the Caregiver Quality of Life Index-Cancer was 88.2. For both patients and caregivers, fulfillment of informational needs regarding side effects and complications (estimates = 0.55, t (16) = 4.88, P < 0.001) and self-care (estimates = 0.73, t (13) = 5.02, P < 0.001) exerted actor effects on their HRQOL, whereas fulfillment of informational needs regarding psychosocial problems (estimates = 0.35, t (13) = 2.90, P = 0.012) exerted a partner effect on the mutual HRQOL.
Conclusions: Multidimensional physio-psychosocial approaches toward patients and their caregivers are important to enhance their HRQOL during the acute phase after HSCT. Detailed overviews of and methods to cope with patients’ psychosocial issues should be provided before discharge, especially for caregivers unable to visit the LTFU clinics.
Introduction
Hematopoietic stem cell transplantation (HSCT), which combines high-dose chemotherapy and/or total body irradiation (TBI) and stem cell infusion, is a treatment that involves a multidisciplinary team for patients with severe hematological diseases1, 2. In Japan, over 5,000 patients undergo HSCT annually3; however, HSCT causes a wide range of physical side effects and complications, including graft-versus-host disease (GVHD), late complications, and secondary cancers4–6. Other side effects include psychological distress5, 7–9, such as anxiety, depression, post-traumatic stress symptoms, fear of recurrence10, 11, and social distress in social participation and returning to work and school12–14. These negatively affect patients' quality of life (QOL), and it is recommended that there should be assessments for health-related QOL (HRQOL) and the management of side effects and complications for survivors who underwent HSCT11.
The majority of studies suggest that over 60% of patients reported good-to-excellent HRQOL at 1-4 years post-HSCT15; however, HRQOL can vary widely between individuals within 1 year post-HSCT16. During hospitalization, the physician and medical staff could intervene in health; however, the opportunity to intervene in health would gradually diminish after discharge from the hospital. Therefore, the Japanese medical center set up long-term follow-up (LTFU) clinics, which support self-care for patients with GVHD and adverse late effects and assessed their HRQOL. In Japan, the mean time in an LTFU clinic is approximately 30 min; however, immediately after discharge, patients need more time to receive information regarding their daily life and medical complications. Therefore, needs assessment is also crucial for evaluating HRQOL and developing the most effective intervention to improve LTFU care.
Moreover, caregivers of patients who undergo HSCT are key people to support their physical, psychosocial, and social care after discharge17–19. The period after discharge is the most precarious for caregivers, as they need to take care of patients alongside their own health would continue for 1 year20. Caregivers encounter various difficulties, such as caregiver burden21, 22 and social and economic problems23, 24. Therefore, exploring caregivers' HRQOL is also essential to consider for patients in homecare. Caregivers also desired to obtain information about late effects and complications of HSCT25 to predict the patients' progress post-HSCT. Caregivers who have more information reveal better HRQOL26. In particular, the transition of care from hospitalization to outpatient care is an important time to understand family dynamics17, 27. Hence, research should include both patients and caregivers and assess the relationships between their needs, specifically informational needs, which is purposed of LTFU clinics and HRQOL.
To the best of our knowledge, few studies have focused on pair analysis in outpatient settings post-HSCT. Such analyses are needed to understand the interactions between patients and their caregivers after discharge from the hospital. Therefore, this study aimed to describe the specific HRQOL of both patients and caregivers and examine the relationship between the fulfillment of informational needs and HRQOL among allo-HSCT recipients and caregivers who visited LTFU clinics within 1.5 years post-HSCT.
Materials and Methods
Study design and participants
We conducted a cross-sectional survey at two university hospitals in Japan between May and December 2018. Patients were considered if aged over 20 years, legally capable of self-determination in Japan, underwent HSCT at research collaboration hospitals, and visited the LTFU clinic at least once within 1.5-year post-HSCT. According to previous guidelines11, patients who undergo HSCT are recommended to be screened at 6 months, 1 year, and then annually. Inclusion criterion was patients with 1.5-year post-HSCT. Caregivers were defined as those aged over 20 years who were most responsible for patient care, regardless of their relationship and living status with the patient. We then excluded the participants whose attending physicians judged them unsuitable for this study considering the patient's medical condition (e.g., relapse of the current disease or severe complications that make it impossible to answer the questionnaire) and a mental status overwhelmed by answering the questionnaire, such as severe depressive symptoms.
Procedure
Patients who met the criteria were chosen by their attending physician or nurses in charge of the LTFU clinic. First, they provided an overview of this study to patients and/or their caregivers. Second, the researchers explained (verbal or written) the details of this study to those who agreed to participate. If caregivers could not visit the hospitals, researchers requested patients to explain this study detail to their caregivers, using a document of the study details. Third, all participants received their questionnaires with their corresponding self-addressed stamped return envelopes, a consent form, and compensation (a gift certificate worth approximately 20 USD). Participants responded to the consent form and the questionnaires within 30 days of receiving them and sent them back to the researchers using their envelopes. Finally, after the questionnaire was administered, researchers obtained the patients' medical data from the medical records of the collaborative hospitals.
Measurements
Patients' HRQOL
We used the Japanese FACT-BMT ver.4.028, which comprises 37 items under five subscales: physical, social or familial, emotional, and functional well-being, and a bone marrow transplant subscale. Higher scores indicated better HRQOL, as calculated using the scoring manual. The FACT-BMT was tested for reliability and validity in Japanese patients who underwent HSCT. The Cronbach's α in this study was 0.86.
Caregivers' HRQOL
We used the Japanese version of the Caregiver Quality of Life Index-Cancer (CQOLC)29, 30, which measures caregivers' HRQOL of patients with cancer and comprises 21 items under four subscales: psychological burden, positive emotions, financial burden, and disruption of daily living. Higher scores indicated better caregivers' HRQOL only by handling psychological burden as reversed scales. The Cronbach's α in this study was 0.87.
Fulfillment of informational needs of patients and caregivers
We created an ad hoc scale to measure the fulfillment of the informational needs participants perceived. First, three professional nurses reviewed the literature and extracted the information that patients and caregivers wanted to know after allo-HSCT. Second, the content and face validity of the questions were confirmed through an interview with four patients who underwent allo-HSCT over 2 years ago and visited the LTFU clinic at least once. Finally, we extracted 52 items and 6 categories (see Appendix), termed general information, post-discharge treatments, side effects and complications, self-care, psychosocial problems, and social resources. If participants did not fill informational needs (participants did not regard an item as unimportant), the item was treated as missing data. The responses of this scale were scored on a five-point Likert scale from 0 (not fulfilled) to 4 (very fulfilled), considering the scoring of the previous research31. We calculated patients' and caregivers' mean scores of the total scores and categorized scores of the fulfillment of informational needs. A higher mean score indicated better fulfillment of needs. Cronbach's α was over 0.90 for both patients and caregivers.
Demographic and medical variables
Patients reported their sex, age, marital status, educational level, economic status, and commuting time to the hospital. Furthermore, caregivers reported their sex, age, relationship to the patient, marital status, health status, educational level, economic status, visiting hours, commuting time to the hospital, and occupation. Family characteristics included the family structure and presence or absence of a related donor in their questionnaires. We also obtained medical data via medical records, such as diagnosis, number of HSCT, graft source, type of HSCT, human leukocyte antigen matching, conditioning regimen, TBI, immunosuppression, GVHD status, engraftment duration, and number of visits to the LTFU clinic.
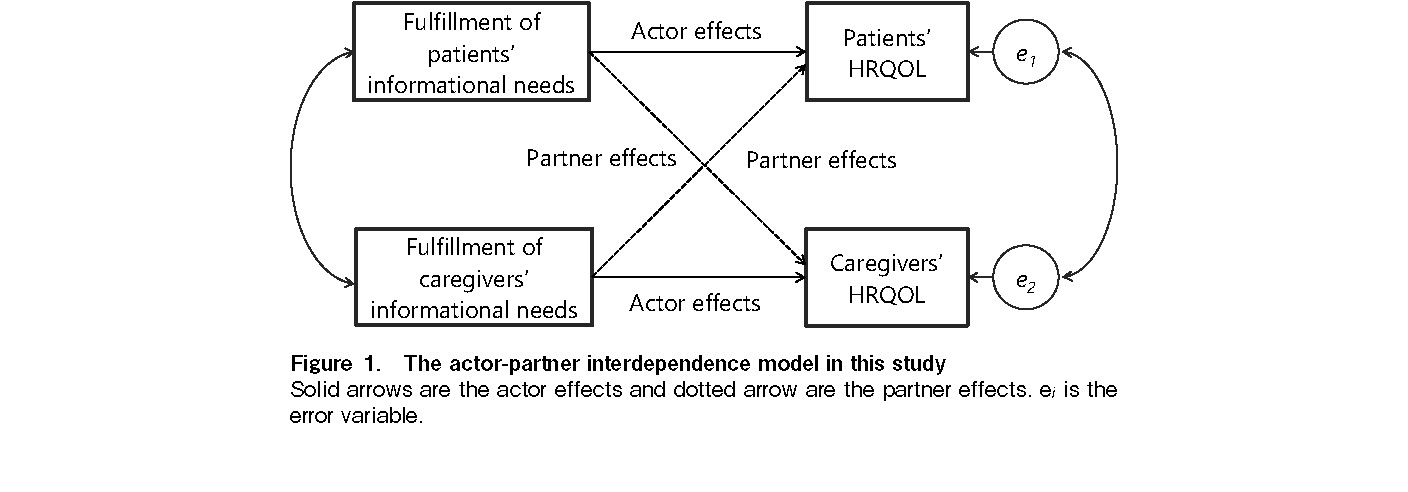
Statistical analysis
We calculated descriptive statistics for the participants' scores to clarify their specific HRQOL. We used a pooled-regression Actor-Partner Interdependence Model (APIM) approach to examine the relationship between participants' fulfillment of informational needs and HRQOL32. The APIM approach frequently uses multilevel modeling and structural equation modeling; however, it might require at least 100 dyads32. The pooled-regression APIM emerged as an alternative statistical approach for use with small sample sizes32. This APIM approach was considered adequate to analyze the dyadic data because it simultaneously estimates the effect of a person's variable (actor effect) and the same variable effect but from the partner (partner effect) on an outcome variable. Considering the outpatient setting, it was important to use dyadic analysis to reflect patient-caregiver relationships (Figure 1).
The homogeneity of variance across levels of the distinguishing variable was tested to examine whether the assumption of this analysis for distinguishable dyads was met before using this APIM approach. This method estimated two regression equations (within- and between-dyad regression) and calculated parameters for actor and partner effects32, 33. First, we calculated the centered scores of the total and subscales of fulfillment of informational needs, then calculated score differences (INdiff) and average scores (INavg) between patients and caregivers. Next, we calculated the standardized HRQOL scores, based on FACT-BMT and CQOLC total scores, and then calculated score differences (QOLdiff) and average scores (QOLavg) between patients and caregivers. Subsequently, we set patients (Gp) as 1 and caregivers (Gc) as −1, and calculated the score differences (Gdiff) (constant term, that is, 2) to confirm the interaction effects. Then, we calculated the products between patients' scores of the fulfillment of informational needs and Gp, and caregivers' scores of the fulfillment of informational needs and Gc, and calculated their score differences to confirm the interactions. Next, we calculated the score differences (INindiff) and average scores (INinavg). Finally, we estimated within-dyad regressions and between-dyad regression as follows (bi = unstandardized regression coefficients, Ei = error terms):
QOLdiff = bw1 (INdiff) + bw2 (Gdiff) + bw3 (INindiff) + Ewi (within-dyad regression)
QOLavg = bb0 + bb1 (INavg) + bb2 (INinavg) + Ebi (between-dyad regression)
Using the unstandardized regression coefficients, we calculated the actor and partner effects using the following equations:
We also calculated the interaction terms of actor and partner effects in similar procedures (informational needs × participants). T-statistics with degrees of freedom were used to determine whether these actor and partner effects differed significantly from zero using the pooled standard errors. We used R ver.3.6.034 and set the p-value as 5% two-tailed.
Ethics considerations
The study was approved by the institutional review board of both hospitals (approval number: 11851-(2) and 30-9-A0620, respectively), where the survey was conducted. Written informed consent was obtained from all participants based on the principles of the Declaration of Helsinki. The researchers explained that participants could withdraw from the study at any time if they disagree to answer the questionnaires. Participants were also instructed not to see each other's questionnaire to avoid the effects from seeing other participants' questionnaire, and to be analyzed as pair.
Results
Participant flow and characteristics
Nineteen patients met the inclusion criteria during the study period; however, one refused to participate. Therefore, 18 patients (with paired caregivers) were recruited. One patient withdrew consent, one patient never visited the LTFU clinic, and two caregivers did not respond to the questionnaire. Finally, 16 patients (response rate: 84%) and 14 caregivers (response rate: 73%) were included in the analysis.
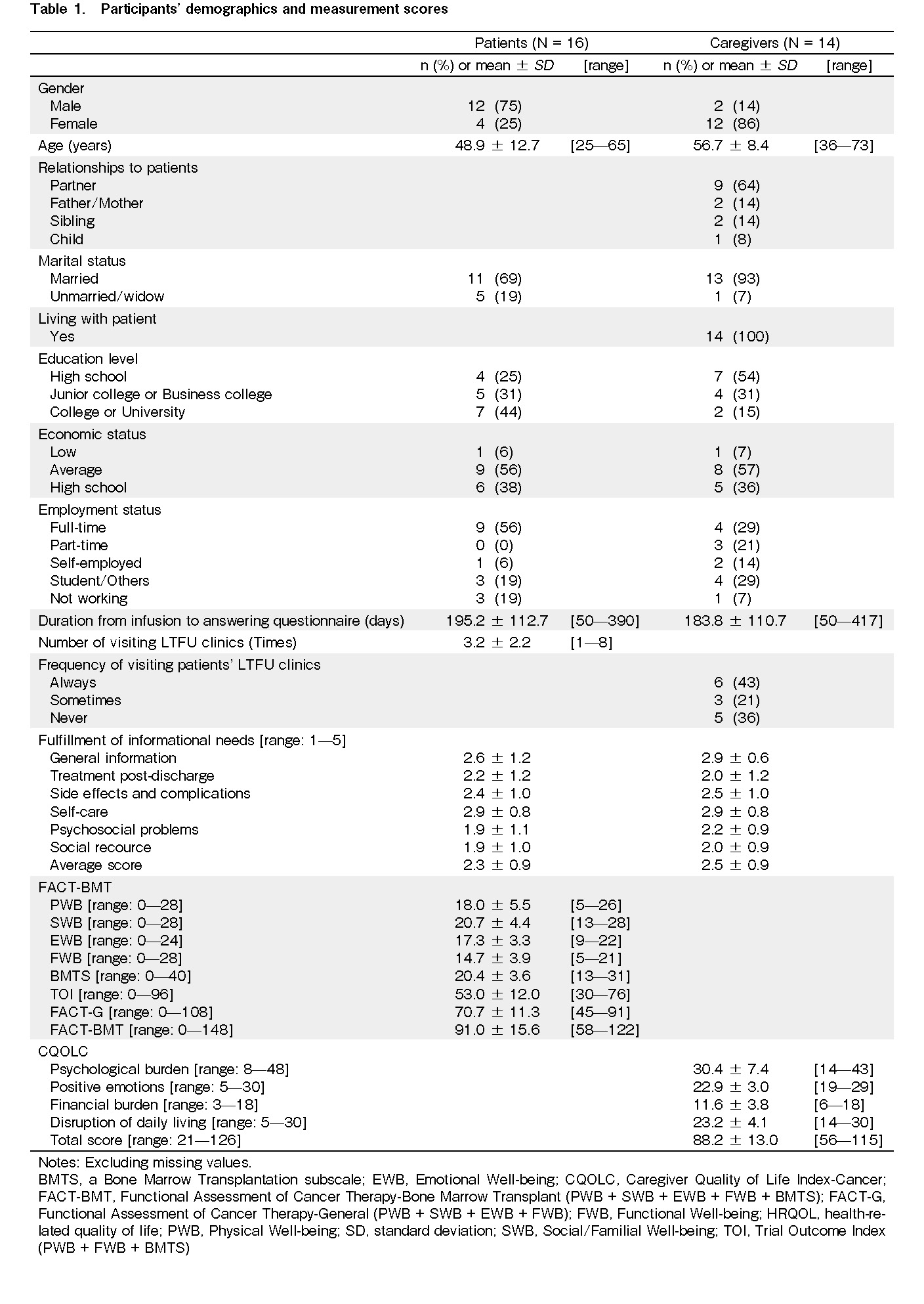
Of the 16 patients, 12 (75%) were male, with a mean age of 48.9 years. The mean duration from the HSC infusion (day 0) to answering the questionnaire was approximately 6.5 months. Patients visited the LTFU clinics approximately 3.2 times on average. Of the 14 caregivers, 12 (86%) were female, with a mean age of 56.7 years. Nine (64%) caregivers were partners, and all caregivers lived with their patients. The mean duration from day 0 to answering the questionnaire was approximately 6 months. Six (43%) caregivers always visited, and three (21%) sometimes visited the LTFU clinic with their patients. The mean total score of the FACT-BMT was 91.0, whereas the mean total score of the CQOLC was 88.2 (Table 1).
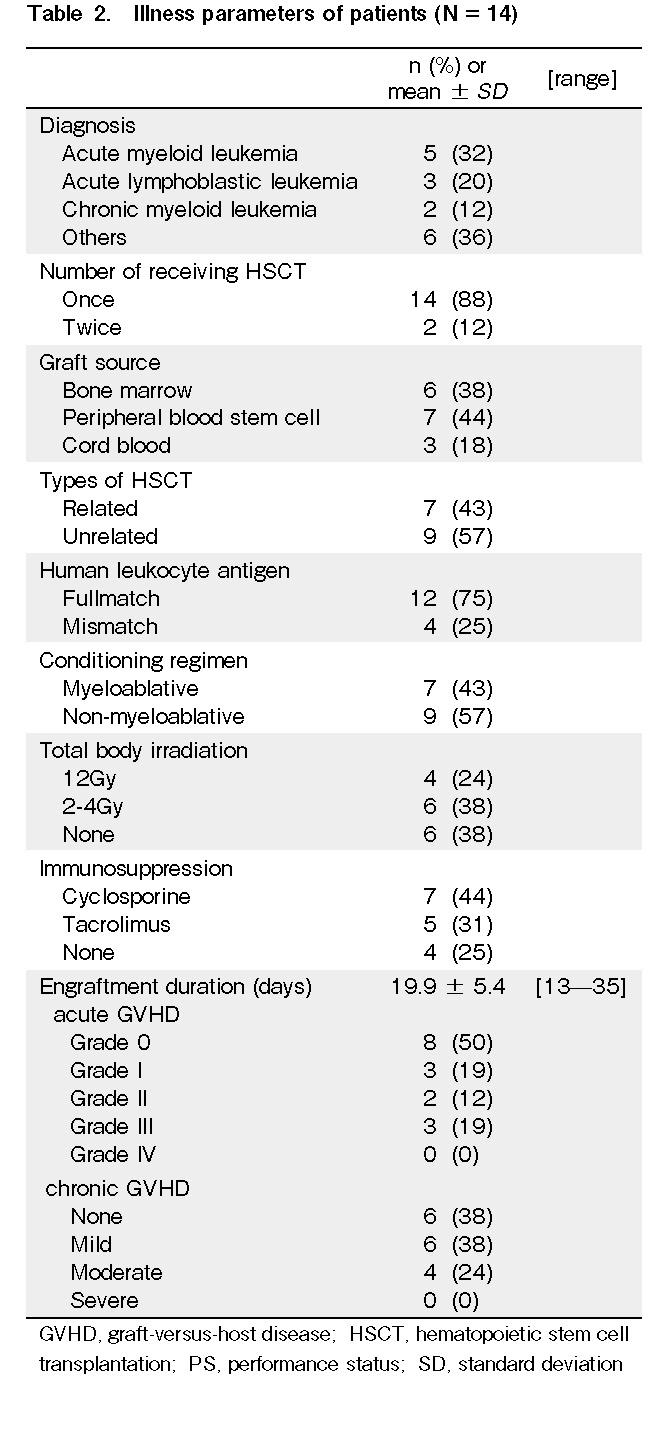
Five (32%) patients were diagnosed with acute myeloid leukemia, and seven (43%) patients received their sibling donor stem cells. Nine (57%) patients received myeloablative conditioning, and 10 (62%) received TBI. The grade of acute GVHD that previously occurred was as follows: grade 0 (n = 8, 50%), grade 1 (n = 3, 19%), grade 2 (n = 2, 12%), and grade 3 (n = 3, 19%), and the grade of chronic GVHD that recently occurred was as follows: none (n = 6, 38%), mild (n = 6, 38%), and moderate (n = 4, 24%). None of the patients had severe chronic GVHD (Table 2).
Relationship between fulfillment of informational needs and HRQOL
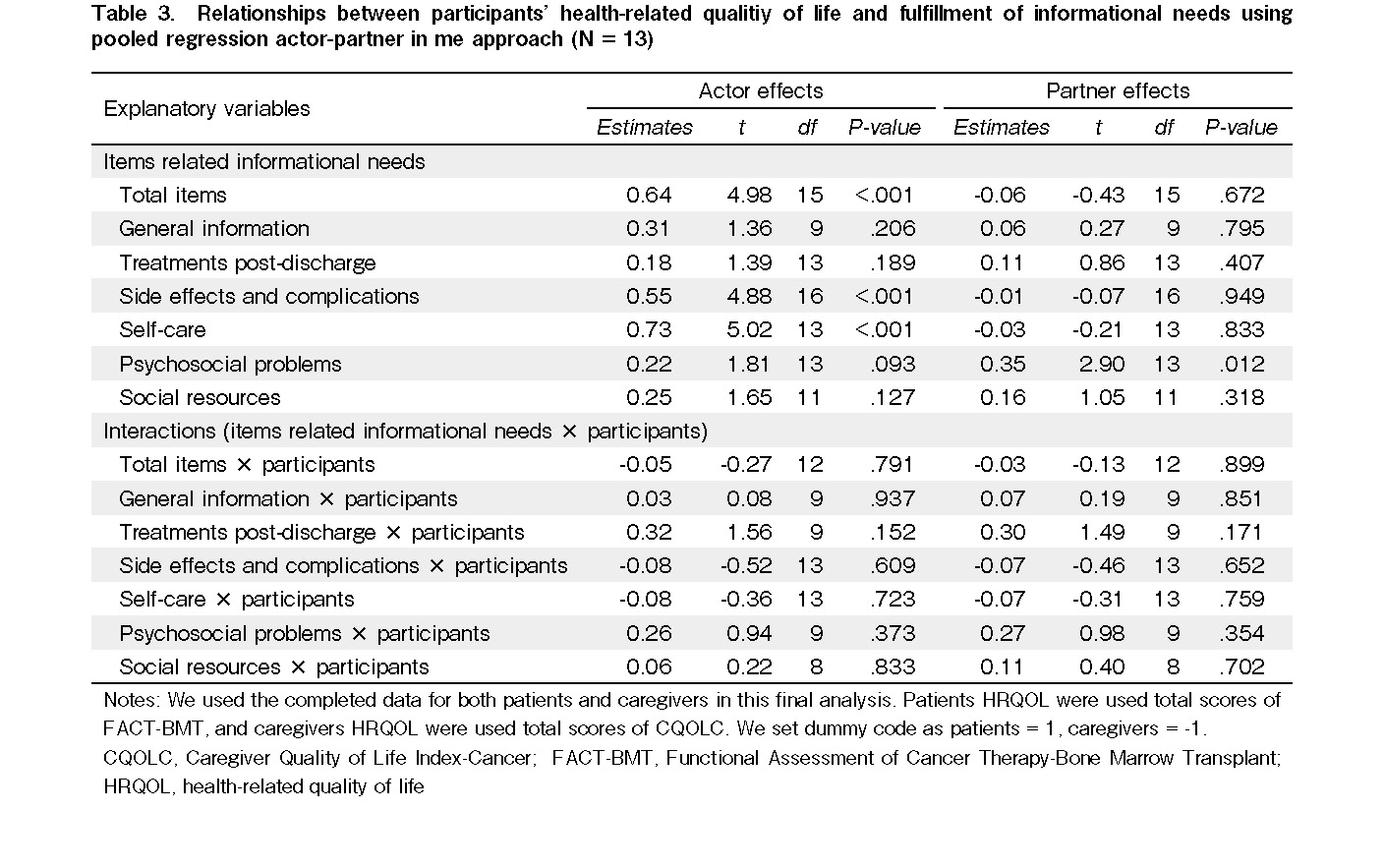
We used the completed data for both patients and caregivers; therefore, 13 pairs were included in the final analysis. All items (estimates = 0.64, t (15) = 4.98, P < 0.001), side effects and complications (estimates = 0.55, t (16) = 4.88, P < 0.001), and self-care (estimates = 0.73, t (13) = 5.02, P < 0.001) exerted actor effects on their HRQOL, whereas fulfillment of informational needs regarding psychosocial problems (estimates = 0.35, t (13) = 2.90, P = 0.012) exerted a partner effect on the mutual HRQOL. Moreover, there were no interactions between the models (items of informational needs × participants) (Table 3).
Discussion
To the best of our knowledge, this is the first study to analyze paired data of post-HSCT patients and their caregivers while focusing on the characteristics of the LTFU clinic. This study investigated specific HRQOL and fulfillment of information needs among patients and caregivers who visited LTFU outpatient clinics within 1.5 years post-HSCT. We examined the relationships using the pooled-regression APIM approach, which indicated that fulfillment of informational needs of all items, side effects, complications, and self-care exerted actor effects on their HRQOL. However, fulfillment of informational needs regarding psychosocial problems exerted a partner effect on mutual HRQOL.
Participants' characteristics
The patients' mean age was consistent with a Japanese nationwide survey3; however, approximately 70% of patients were men in this study. The effect of the sex ratio of the patients should be considered with caution. In addition, most patients received a non-myeloablative conditioning regimen, which has a lower risk of chronic GVHD than a myeloablative regimen6. Chronic GVHD usually occurs approximately 3-15 months post-HSCT6, indicating that few patients had moderate and severe GVHD.
In this study, most caregivers were women and spouses or partners, consistent with previous studies22, 26, 35–39. This bias of sex and relationship among caregivers was considered with caution. Approximately 60% of caregivers attended the patient's LTFU clinic visit every time or occasionally, indicating that assessment and intervention for the caregivers in the LTFU clinic are also necessary for the acute phase after discharge.
Participants' specific HRQOL
Patients' functional well-being (FWB) scores were higher than those in a previous study (score = 11.1) after exiting the cleanroom post-HSCT in Japan40. In a previous study, the FWB score focused on housework or activity and increased over time41. Also, previous prospective study indicated that 20% of participants returned to full-time work by a year, and return to work was significantly delayed for women42. The patients in this study were predominantly men, and it is thought that their activity status improved due to their return to work, school, or their lifestyle change at home following discharge from the hospital. Thus, their FWB was higher than that when they left the cleanroom. However, patients' social or familial well-being scores were lower than those in a previous study (score = 23.8)40, which was consistent with a decrease over time in a previous longitudinal study41. This is because patients could be infectious because of their vulnerable immune system10 and have little time to interact with their friends and family members43, 44. Thus, we should support not only patients' GVHD and its side effects but also social and familial relationships in LTFU clinics.
Caregivers' total score and all subscales of CQOLC were higher than those of caregivers with advanced cancer patients (total and subscale scores including included psychological burden, positive emotions, financial burden, and disruption of daily living are 71.8, 27.3, 17.6, 9.1, and 17.9, respectively)29. Patients in this study had less incidence of GVHD and better performance status. A previous study indicated that caregivers' lower burden scores correlated with caregivers' higher HRQOL22. Moreover, female caregiver burdens tend to be higher than those of male21. Thus, caregivers in this study indicated better specific HRQOL than those in a previous study.
Relationships between patients' and caregivers' HRQOL and fulfillment of informational needs
Side effects, complications, and self-care as explanatory variables exerted actor effects on their HRQOL, consistent with a previous study45 on hematological cancer patients and another46 on caregivers of patients with cancer. Most patients who received allo-HSCT reported physical problems within 1 year47, and patients and caregivers recognized that these problems were most important after discharge. The fulfillment of these key informational needs, such as post-treatment complications and conditioning treatment, measures to prevent infections, and management of daily life after discharge, would improve HRQOL for both patients and caregivers.
However, psychosocial problems as explanatory variables exerted a partner effect on mutual HRQOL. The subscales of side effects, complications, and self-care, which were significantly related to HRQOL in actor effect, focused on patients' problems. In contrast, this subscale of psychosocial problems, which is significantly related to HRQOL in partner effect, focused on family and social problems. Patients who received HSCT were concerned about family members and the workplace38, 44. A previous study48 reported that patients struggled with these concerns, then coped with not expressing their distress to their caregivers. These coping mechanisms indicated lower HRQOL in patients. Enhancing patients' fulfillment of informational needs on psychosocial problems was regarded as supporting family and problems. Therefore, open communication might enhance mutual HRQOL.
Implications for clinical practice
Healthcare providers should understand that patients' social well-being is diminished after hospital discharge. A previous cross-sectional study41 also showed that patients were concerned about their jobs, finances, and relations in the period after discharge. Health care providers should also consider assessing social aspects, such as caregivers, family members, friends, and workplaces of the patient. Therefore, it is important to assess these factors during hospitalization. Healthcare providers also noticed that they had less access to caregivers after the patients were discharged. Although some caregivers may attend the LTFU outpatient clinic, it is necessary to evaluate and support the role and social aspects of caregivers during hospitalization.
Moreover, health care providers should intervene to satisfy informational needs of caregivers and patients regarding medical complications and self-care. Considering the purposes of LTFU clinics, health care providers support patients' social and familial relationships, which can improve the general condition of patients. For example, presenting appropriate social resources and listening to caregivers' conditions would be effective for patients in the acute phase after discharge. Furthermore, health care providers should understand that patients' and caregivers' needs would change49. A previous study reported that it is important that nurses assess the overall well-being of patients and caregivers to enhance coping and problem-solving skills of the HSCT process50. If caregivers did not attend the LTFU clinic, health care providers should assess the patients' psychosocial needs and support and unmet informational needs, mutually enhancing their HRQOL.
Limitations
First, this cross-sectional observational study did not clarify the causal relationship between participants' fulfillment of informational needs and HRQOL. We also could not consider the trajectory of the participants' HRQOL and informational needs. Moreover, the small sample size could reduce the statistical power. Further studies should include more participants, predominantly female patients and male caregivers, and adjust variables related to participants' specific HRQOL, such as using longitudinal studies and structural equation modeling. Second, in the pooled-regression APIM approach, we set participants' specific HRQOL as the outcome variable. However, the construction concepts of these variables were not similar; thus, we should pay attention to the proper interpretation of this result. Lastly, the system of the LTFU clinic at the research cooperating facilities might be different, such as staff and resources. Further studies should consider using multilevel analyses among facilities.
In conclusion, physio-psychosocial approaches toward patients and their caregivers are important to enhance their HRQOL during the acute phase after HSCT. Detailed overviews of and methods to cope with patients' psychosocial issues should be provided before discharge, especially for caregivers unable to visit the LTFU clinics.
Acknowledgments
We would like to thank the patients, caregivers, and family members for taking time out of their busy schedules to participate in this study. We are grateful to Dr. Yosuke Masamoto, Dr. Koji Kobayashi, Ms. Satoko Nakano, Ms. Shinobu Nakanishi, and Ms. Sumie Isono for their collaboration in data collection. We received generous support and advice from Ms. Reiko Yamahana and Ms. Chika Yoshida on the measurements used in this study. We also thank all medical professionals at the collaborating institutions.
Author Contributions
SN contributed to the conception and design of the study, data collection, data analysis, and manuscript drafting, and KK supervised the entire study process and critically reviewed the manuscript. All authors read and approved the final manuscript.
Conflicts of Interest
The authors declare no conflict of interest. This study was supported by a grant-in-aid from “YAMAJI FUMIKO NURSING RESEARCH FUND” in 2018 (PI: Shohei Nakajima). Disclosure forms provided by the authors are available on the website.
References
1.Copelan EA. Hematopoietic stem-cell transplantation. N Engl J Med. 2006; 354: 1813-26.
2.Inamoto Y, Lee SJ. Late effects of blood and marrow transplantation. Haematologica. 2017; 102: 614-25.
3.The Japan Data Center for Hematopoietic Cell. Activities and Outcomes of Hematopoietic Cell Transplantation in Japan (2018). JDCHCT. Available from:
4.Barata A, Wood WA, Choi SW, Jim HSL. Unmet needs for psychosocial care in hematologic malignancies and hematopoietic cell transplant. Curr Hematol Malig Rep. 2016; 11: 280-7.
5.Jim HSL, Sutton SK, Jacobsen PB, Martin PJ, Flowers ME, Lee SJ. Risk factors for depression and fatigue among survivors of hematopoietic cell transplantation. Cancer. 2016; 122: 1290-7.
6.Kanda J, Nakasone H, Atsuta Y, Toubai T, Yokoyama H, Fukuda T, et al. Risk factors and organ involvement of chronic GVHD in Japan. Bone Marrow Transplant. 2014; 49: 228-35.
7.El-Jawahri AR, Vandusen HB, Traeger LN, Fishbein JN, Keenan T, Gallagher ER, et al. Quality of life and mood predict posttraumatic stress disorder after hematopoietic stem cell transplantation. Cancer. 2016; 122: 806-12.
8.Kenzik K, Huang IC, Rizzo JD, Shenkman E, Wingard J. Relationships among symptoms, psychosocial factors, and health-related quality of life in hematopoietic stem cell transplant survivors. Support Care Cancer. 2014; 23: 797-807.
9.Sarkar S, Scherwath A, Schirmer L, Schulz-Kindermann F, Neumann K, Kruse M, et al. Fear of recurrence and its impact on quality of life in patients with hematological cancers in the course of allogeneic hematopoietic SCT. Bone Marrow Transplant. 2014; 49: 1217-22.
10.Hilgendorf I, Greinix H, Halter JP, Lawitschka A, Bertz H, Wolff D. Long-term follow-up after allogeneic stem cell transplantation. Dtsch Arztebl Int. 2015; 112: 51-8.
11.Majhail NS, Rizzo JD, Lee SJ, Aljurf M, Atsuta Y, Bonfim C, et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation. Bone Marrow Transplant. 2012; 47: 337-41.
12.Bevans M, El-jawahri A, Tierney DK, Wiener L, Wood WA, Hoodin F, et al. Biology of blood and marrow transplantation National Institutes of Health Hematopoietic Cell Transplantation Late Effects Initiative : the Patient-Centered Outcomes Working Group Report. Biol Blood Marrow Transplant. 2017; 23: 538-51.
13.Brice L, Gilroy N, Dyer G, Kabir M, Greenwood M, Larsen S, et al. Haematopoietic stem cell transplantation survivorship and quality of life: is it a small world after all? Support Care Cancer. 2017; 25: 421-7.
14.Cooke L, Grant M, Gemmill R. Discharge needs of allogeneic transplantation recipients. Clin J Oncol Nurs. 2012; 16: E142-9.
15.Pidala J, Anasetti C, Jim H. Quality of life after allogeneic hematopoietic cell transplantation. Blood. 2009; 114: 7-19.
16.Jim HSL, Sutton SK, Small BJ, Jacobsen PB, Wood WA, Knight JM, et al. Trajectories of quality of life after hematopoietic cell transplantation: secondary analysis of blood and marrow transplant clinical trials network 0902 data. Biol Blood Marrow Transplant. 2016; 22: 2077-83.
17.Langer S, Lehane C, Yi J. Patient and caregiver adjustment to hematopoietic stem cell transplantation: a systematic review of dyad-based studies. Curr. Hematol. Malig. Rep. 2017; 12: 324-34.
18.Tichelli A, Rovó A. Survivorship After Allogeneic Transplantation―Management Recommendations for the Primary Care Provider. Curr. Hematol. Malig. Rep. 2015; 10: 35-44.
19.Wulff-Burchfield EM, Jagasia M, Savani BN. Long-term follow-up of informal caregivers after allo-SCT: a systematic review. Bone Marrow Transplant. 2013; 48: 469-73.
20.Sabo B, McLeod D, Couban S. The experience of caring for a spouse undergoing hematopoietic stem cell transplantation: opening Pandora's box. Cancer Nurs. 2013; 36: 29-40.
21.Akgul N, Ozdemir L. Caregiver burden among primary caregivers of patients undergoing peripheral blood stem cell transplantation: a cross sectional study. Eur J Oncol Nurs. 2014; 18: 372-7.
22.Deniz H, Inci F. The burden of care and quality of life of caregivers of leukemia and lymphoma patients following peripheric stem cell transplantation. J Psychosoc Oncol. 2015; 33: 250-62.
23.Simoneau TL, Mikulich-Gilbertson SK, Natvig C, Kilbourn K, Spradley J, Grzywa-Cobb R, et al. Elevated peri-transplant distress in caregivers of allogeneic blood or marrow transplant patients. Psychooncology. 2013; 22: 2064-70.
24.Denzen EM, Thao V, Hahn T, Lee SJ, McCarthy PL, Rizzo JD, et al. Financial impact of allogeneic hematopoietic cell transplantation on patients and families over 2 years: Results from a multicenter pilot study. Bone Marrow Transplant. 2016; 51: 1233-40.
25.Sirilla J, Overcash J. Quality of life (QOL), supportive care, and spirituality in hematopoietic stem cell transplant (HSCT) patients. Support Care Cancer. 2013; 21: S1137-44.
26.Cooke L, Grant M, Eldredge DH, Maziarz RT, Nail LM. Informal caregiving in hematopoietic blood and marrow transplant patients. Eur J Oncol Nurs. 2011; 15: 500-7.
27.Siminoff LA, Zyzanski SJ, Rose JH, Zhang AY. The Cancer Communication Assessment Tool for Patients and Families (CCAT-PF): a new measure. Psychooncology. 2008; 17: 1216-24.
28.Imataki O, Nakajima K, Inoue N, Tamai Y, Kawakami K. Evaluation of QOL for stem cell transplantation recipients by SF-36 and FACT-BMT: preliminary results of FACT-BMT for Japanese patients. Japanese J Cancer Chemother. 2010; 37: 847-51.
29.Ando S, Harada M, Michael AW, Kuji M, Shimizu M, Sato K, et al. Reliability and validity of Japanese version Caregiver Quality of Life Index−Cancer (CQOLC). Palliat Care Res. 2013; 8: 286-92. (in Japanese)
30.Weitzner MA, Jacobsen PB, Wagner H, Friedland J, Cox C. The Caregiver Quality of Life Index-Cancer (CQOLC) scale: development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Qual Life Res. 1999; 8: 55-63.
31.Schur S, Neubauer M, Amering M, Ebert-Vogel A, Masel EK, Sibitz I, et al. Validation of the Family Inventory of Needs (FIN) for family caregivers in palliative care. Palliat Support Care. 2013; 13: 485-91.
32.Tambling RB, Johnson SK, Johnson LN. Analyzing dyadic data From small samples. Couns Outcome Res Eval. 2011; 2: 101-14.
33.Kenny DA, Kashy DA, Cook WL. Dyadic Data Analysis. New York, London, The Guilford Press, 2006
34.R Core Team. R: The R Project for Statistical Computing. Available from:
35.Beattie S, Lebel S, Petricone-Westwood D, Wilson KG, Harris C, Devins G, et al. Balancing give and take between patients and their spousal caregivers in hematopoietic stem cell transplantation. Psychooncology. 2017; 26: 2224-31.
36.Fife BL, Monahan PO, Abonour R, Wood LL, Stump TE. Adaptation of family caregivers during the acute phase of adult BMT. Bone Marrow Transplant. 2009; 43: 959-66.
37.Jamani K, Onstad LE, Bar M, Carpenter PA, Krakow EF, Salit RB, et al. Quality of life of caregivers of hematopoietic cell transplant recipients. Biol Blood Marrow Transplant. 2018; 24: 2271-6.
38.Poloméni A, Lapusan S, Bompoint C, Rubio MT, Mohty M. The impact of allogeneic-hematopoietic stem cell transplantation on patients' and close relatives' quality of life and relationships. Eur J Oncol Nurs. 2016; 21: 248-56.
39.Posluszny DM, Bovbjerg DH, Agha ME, Hou JZ, Raptis A, Boyiadzis MM, et al. Patient and family caregiver dyadic adherence to the allogeneic hematopoietic cell transplantation medical regimen. Psychooncology. 2018; 27: 354-8.
40.Harada M, Nakamura M. The change of QOL after transplantation in allogeneic hematopoietic stem cell transplant patients. Yamanashi Nurs J. 2009; 8: 15-22. (in Japanese)
41.McQuellon RP, Russell GB, Rambo TD, Craven BL, Radford J, Perry JJ, et al. Quality of life and psychological distress of bone marrow transplant recipients: The ‘time trajectory' to recovery over the first year. Bone Marrow Transplant. 1998; 21: 477-86.
42.Syrjala KL, Langer SL, Abrams JR, Storer B, Sanders JE, Flowers MED, et al. Recovery and Long-term Function After Hematopoietic Cell Transplantation for Leukemia or Lymphoma. JAMA 2004; 291: 2335.
43.Bergkvist K, Larsen J, Johansson UB, Mattsson J, Fossum B. Family members' life situation and experiences of different caring organisations during allogeneic haematopoietic stem cells transplantation−a qualitative study. Eur J Cancer Care (Engl). 2018; 27: e12610.
44.Niederbacher S, Them C, Pinna A, Vittadello F, Mantovan F. Patients' quality of life after allogeneic haematopoietic stem cell transplantation: mixed-methods study. Eur J Cancer Care (Engl). 2012; 21: 548-59.
45.Rood JAJ, van Zuuren FJ, Stam F, van der Ploeg T, Eeltink C, Verdonck-de Leeuw IM, et al. Perceived need for information among patients with a haematological malignancy: Associations with information satisfaction and treatment decision-making preferences. Hematol Oncol. 2015; 33: 85-98.
46.Fridriksdóttir N, Sævarsdóttir P, Halfdánardóttir SÍ, Jónsdóttir A, Magnúsdóttir H, Ólafsdóttir KL, et al. Family members of cancer patients: needs, quality of life and symptoms of anxiety and depression. Acta Oncol (Madr). 2011; 50: 252-8.
47.Braamse AMJ, Van Meijel B, Visser O, Huijgens PC, Beekman ATF, Dekker J. Distress, problems and supportive care needs of patients treated with auto-or allo-SCT. Bone Marrow Transplant. 2014; 49: 292-8.
48.Langer SL, Brown JD, Syrjala KL. Intrapersonal and interpersonal consequences of protective buffering among cancer patients and caregivers. Cancer. 2009; 115: 4311-25.
49.Gemmill R, Cooke L, Williams AC, Grant M. Informal caregivers of hematopoietic cell transplant patients: A review and recommendations for interventions and research. Cancer Nurs. 2011; 34: E13-21.
50.Çuhadar D, Tanriverdi D, Pehlivan M, Kurnaz G, Alkan S. Determination of the psychiatric symptoms and psychological resilience levels of hematopoietic stem cell transplant patients and their relatives. Eur J Cancer Care (Engl). 2016; 25: 112-21.
Search
News