Volume 4 (2021) Issue 3 No.1 Pages 48-53
Abstract
Background :There is a lack of prospective studies to address the issue of timing of bone mineral density (BMD) measurement and anti-resorptive therapy before and after allogeneic hematopoietic cell transplantation (allo-HCT), specifically in the younger population (age < 40 years). This study evaluated the incidence and risk factors of poor BMD in young Indian patients undergoing allogeneic hematopoietic cell transplant and the effect of anti-resorptive therapy in allogeneic transplant recipients who are at high risk for severe bone loss.
Methods :This was a single-center, prospective study conducted from 2016 to 2019. All patients aged ≥ 12 years undergoing allo-HCT were included in the study. Data regarding the risk factors for osteoporosis, underlying diagnoses, and HCT characteristics were recorded. BMD was measured by dual-energy X-ray absorptiometry (DXA) (HOLOGIC Discovery A) at the lumbar spine (LS), femoral neck (FN), and total hip (TH) at pre-HCT, day+100, and day+365 post-HCT. Patients with Z-score ≤ -2 at day+100 were given one dose (4 mg) of intravenous zoledronate. Patients with moderate to severe chronic graft-versus-host disease (GVHD) also received a dose of zoledronate if they had not received it earlier.
Results :The median age of our cohort was 24 years (IQR 18.5 – 39.5). Day+100 DXA was available for 25 (54.3%) patients, a paired day+100, and day+365 DXA was available for 15 patients. For pre-HCT, a Z-score ≤ -2 was seen in 30% of patients. For day+100 post-HCT, a Z-score ≤ -2 was seen in 44% of patients. Low body mass index was associated with a Z-score ≤ -2 (median 18 vs. 23 kg/m2, P = 0.04). Despite a single dose of zoledronate in this cohort, the median Δ BMD (day+365 – day+100) loss at FN and LS was -0.8% to -3.7%, respectively. Seven (64%) of these patients also had moderate-severe chronic GVHD.
Conclusions :BMD below the expected range for age (Z-score ≤ -2) was present in one-third of young Indian patients undergoing allo-HCT in this single center study. Without intervention, up to half of the patients had a Z-score ≤ -2 at day+100 post-HCT. BMD loss at day+100 persisted at day+365 despite anti-resorptive therapy.
Introduction
The American Society for Transplantation and Cellular Therapy (ASTCT) expert panel opinion has recently updated their guidance on the management of bone health after hematopoietic cell transplantation (HCT) based on evidence derived from retrospective HCT studies, results extrapolated from prospective studies in non-HCT settings, and societal guidelines1. They advise BMD measurement pre-HCT in patients with high-risk factors and at 3-months post-HCT if measurement is not done pre-HCT1. As per the previous recommendation, dual-energy X-ray absorptiometry (DXA) was done at 1-year post-transplant and at earlier time points in patients with GVHD and steroid use2. These recommendations were based on observations that suggested that nadir bone mineral density (BMD) loss occurred at six months to one year3,4. However, a few studies have indicated that BMD loss may occur earlier than six months and as early as three months post-HCT5,6. Recently, the International Osteoporosis Foundation Working Group on Cancer and Bone Disease also recommended DXA at 3-months post-HCT7. Although there is an evolving consensus on when to do DXA scans, there is no consensus on the timing for pharmacologic intervention based on T-score/Z-score cutoffs or percentage BMD loss in the younger population (age < 40 years) in the post-HCT setting3,6. The ASTCT guidance proposes starting pharmacologic therapy in those < 40-years of age receiving prednisone equivalent doses of ≥ 7.5 mg/day for ≥ 6 months and either exhibiting fragility fractures, Z-score < -3.0, or 10% BMD loss over a year1. The Indian population has a lower BMD compared to the Caucasian population8. The prevalence of osteoporosis is also higher in the Indian population compared to other ethnicities9. India's only cross-sectional study showed that femoral neck BMD was significantly lower than age, gender, and body mass index-matched controls beyond 2-years post HCT10. The primary objective of this study was to prospectively evaluate the incidence of low BMD and the affecting factors at pre-HCT, day+100, and one-year post HCT in young Indian patients undergoing allogeneic HCT. The secondary objective was to evaluate the effect of administration of anti-resorptive therapy in patients who were at a high risk of developing accelerated bone loss in the post-HCT period.
Patients and Methods
This was a single-center, prospective study conducted from 2016 to 2019.
Inclusion criteria: All patients above the age of 12 years undergoing allogeneic transplantation were included in this study. Patients were eligible regardless of the basic diagnosis, donor source, or intensity of the conditioning regimen.
Ethical considerations: The study was approved by the Institutional Ethics Committee, and written informed consent was obtained from all study participants.
Objectives of the study: (1) to study the incidence and risk factors for low BMD (Z-score
BMD measurement: BMD was measured by DXA using the HOLOGIC Discovery A machine in accordance with the manufacturer recommendations and International Society for Clinical Densitometry (ISCD) guidance11. BMD was measured at the lumbar spine (LS), femoral neck (FN), and total hip (TH). Quality control assessments were done every day using an internal calibration step and an external anthropomorphic spine phantom scan according to the manufacturer's recommendations. As most patients in our cohort were pre-menopausal women and men aged <50-years, we used Z-score cutoffs of -2.0 or lower to define
Transplantation procedure: Detailed data about demographics, anthropometry, nutrition, and risk factors for osteoporosis11, underlying diagnoses, transplantation details, graft versus host disease (GVHD), endocrine, and drugs that affect BMD were recorded. All patients received cyclosporine as a part of GVHD prophylaxis. All patients were prescribed supplemental calcium of 1,000 mg/day and vitamin D of 1,000 IU per day. In patients with vitamin D levels less than 30 ng/mL at baseline or anytime during follow-up, they were given a vitamin D of 600,000 units stat dose under supervision. Patients were counseled regarding maintaining a diet adequate for caloric and protein intake and maintaining a lifestyle that included weight-bearing exercises three times a week.
Study interventions: Patients with Z-score
Statistical analysis: For statistical analysis, continuous variables are expressed as median (interquartile range), and categorical variables are expressed as proportions (percentages). The two groups were compared by t-test and chi-square test. A P < .05 was considered statistically significant.
Results
A total of 58 patients above 12 years underwent allogeneic HCT during the period 2016 – 2019. There were 12 deaths before day+100. DXA was available for 25 patients by day+100 (25/46, 54.3%). The median age for our cohort was 24 years (IQR 18.5 – 39.5). Of the 12 female patients in the cohort, only one was post-menopausal at the time of transplant. Between day+100 and day+365, there were four more deaths, and DXA was unavailable in six more patients. Therefore, paired day+100 and day+365 DXA were available for 15 patients (15/21, 71.4%). Pre-HCT DXA was available for another cohort of 20 patients.
BMD was below the expected range for age as early as day+100 post-HCT
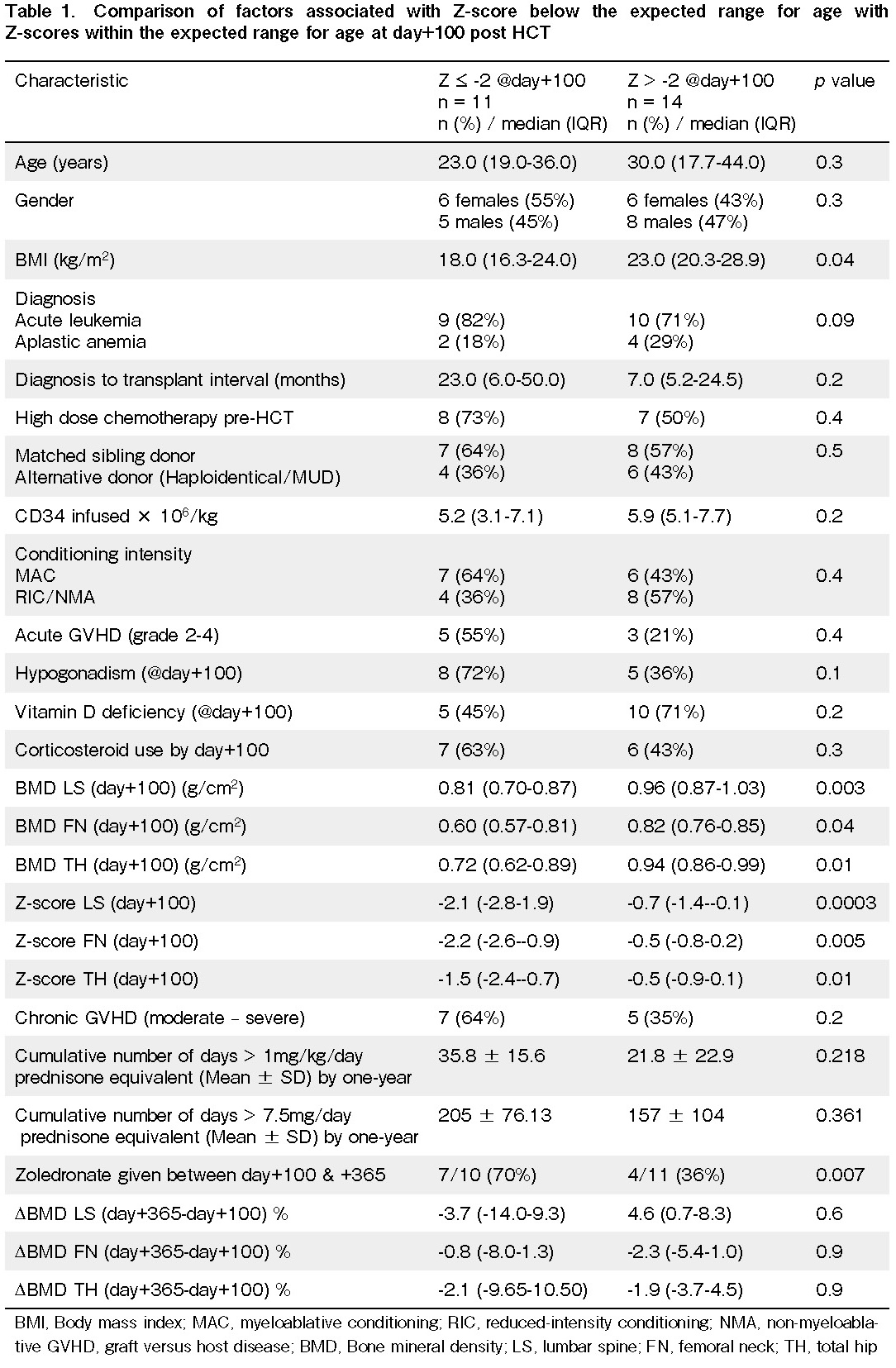
A total of 11 (44%) patients had Z-scores ≤ -2.0 by day+100. The median Z-scores at LS, FN, and TH in this cohort of patients were -2.1, -2.2, and -1.5, respectively, compared to -0.7, -0.5, and -0.5, respectively, in the cohort with Z-scores within the expected range for age. The median BMD was lowest at the FN, and this was followed by TH and LS. The median BMD was also significantly lower in the cohort with Z-score ≤ -2 (0.607, 0.717, 0.810 gm/cm2, respectively) than it was in patients in the cohort with Z-score > -2 (0.819, 0.937, 0.964 gm/cm2, respectively) (P < 0.01) (Table 1). While examining the two groups' clinical variables only BMI was significantly different between those with Z-scores below and above -2 (median 18 vs. 23 kg/m2, P = 0.04). Age, gender, diagnosis, diagnosis to transplant interval, donor source, high dose chemotherapy before HCT, myeloablative conditioning regimen, CD34 dose infused, vitamin D deficiency, acute GVHD (grade 2-4 requiring systemic steroids), and hypogonadism at day+100 were not significantly different between the two cohorts.
BMD loss at day+100 persisted at day+365 despite anti-resorptive therapy
Patients with Z-score ≤ -2.0 and patients with moderate-severe chronic GVHD received a single dose of intravenous zoledronate 4 mg once between day+100 and day+365 (70% vs. 36%, P = 0.007) (Table 1). There were no major adverse events reported after zoledronate infusion. Despite the administration of Zoledronate to high risk patients, the Δ BMD (day+365 – day+100) had a median loss of -0.8% to -3.7% at FN and LS, respectively, in the cohort with Z-score ≤ -2.0 compared to loss of -2.3% to +4.6% in the cohort with Z-score > -2.0 (P = 0.6). None of the patients had any pathological fracture or additional bone health issues within one-year post-HCT.
BMD loss was present even before HCT
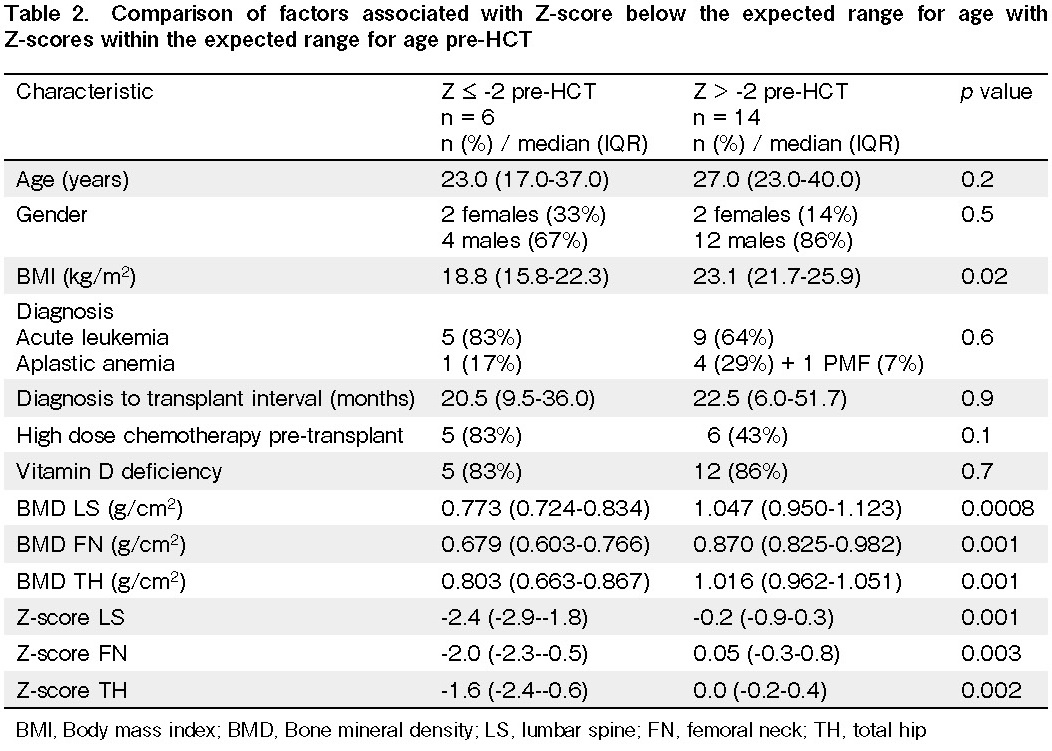
A total of 6/20 (30%) patients had Z-scores ≤ -2.0 pre-HCT. These patients had median Z-scores of -2.4, -2.0, and -1.6 and BMD of 0.773, 0.679, and 0.803 at LS, FN, and TH, respectively. The other cohort with BMD within the expected range for age had Z-scores of -0.2, 0.05, 0.0, and BMD of 1.047, 0.870, and 1.016, respectively (Table 2). Again, low BMI (18.8 vs. 23.1 kg/m2, P = 0.02) was the only factor associated with low BMD. The remaining factors were not significantly different between the two cohorts.
Discussion
Few studies have looked at early BMD loss post-HCT around day+100 and have reported an osteopenia (T-score < -1 and > -2.5)/osteoporosis (T-score ≤ -2.5) at a combined rate of 48% to 68%5,6. Both of these studies used the WHO definition for reporting BMD, as they were published before the recent ISCD official position on reporting BMD in the younger population that recommended the use of Z-scores12. The median age in these studies was 41 years and 51 years, respectively. Our cohort was much younger, with a median age of 24 years. Despite the differences in BMD terminology, patients in our cohort had a near equivalent incidence (44%) of BMD below the expected range for age (Z-score ≤ -2). Only one of the above studies looked at pre-HCT BMD and reported the prevalence of osteopenia/osteoporosis to be 53%6. In our study, 30% of the patients had a Z-score ≤ -2 pre-HCT. Our study found that only low BMI was associated with a Z-score ≤ -2. Most other risk factors described previously to affect BMD were not significant in our study, probably due to the small number of patients 14,14. Given the high prevalence of low BMD pre-HCT and at day+100 post-HCT, we agree with the recent ASTCT and International Osteoporosis Foundation recommendations to screen all patients undergoing allo-HCT with a DXA scan at pre-HCT or at day+100 if not done pre-HCT1,7 rather than restricting early screening to only patients with GVHD and steroid use2.
While there is no consensus on the T-score cutoffs for pharmacologic intervention when the T-score is < -1 and > -2.5, the International Osteoporosis Foundation recommends a T-score < -1.57. In contrast, others recommend a T-score ≤ -1 in patients with risk factors or a high FRAX score4. Although ASTCT guidance proposes pharmacologic therapy in patients < 40-years of age receiving a prednisone equivalent dose of ≥ 7.5 mg/day for ≥ 6 months and either one of fragility fractures or Z-score < -3.0 or 10% BMD loss over a year, the evidence for this method is lacking1. In our study, we gave zoledronate to patients with Z-scores ≤ -2, which are below the expected range for age or patients with a risk factor of moderate-severe chronic GVHD that requires prolonged corticosteroid therapy. However, this approach could stop further BMD loss, and it could not recover the early loss that occurred at day+10015. This suggests that some patients with ongoing risk factors might be candidates for repeated anti-resorptive therapy. The major limitations of our study are the small sample size, the lack of serial pre-HCT and post-HCT BMD, the use of HOLOGIC reference standards, and missing data (due to deaths and unavailability of DXA), which reflect real-world challenges in ensuring adherence to bone health surveillance after HCT in resource-limited settings4. Large prospective multicenter studies are needed to fill the lacunae in understanding the BMD loss post-HCT. While serial BMD testing with bone turnover markers can be used to determine the time to initiate therapy16, only an RCT can address the benefit of early intervention in the younger population (CTRI/2019/04/018764). Until then, we propose starting anti-resorptive therapy in young patients with a Z-score ≤ -2 and repeating a dose in those with ongoing risk factors for bone loss.
Author Contributions
NSK, AS, SB, PM, and DPL conceived the study, drafted the manuscript, and approved the final version. All authors contributed to patient care. DPL and NSK confirm full access to the data in the study and accept the final responsibility for the manuscript.
Conflicts of Interest
The authors declare no conflict of interest. Disclosure forms provided by the authors are available on the website.
References
1.Bar M, Ott SM, Lewiecki EM, Sarafoglou K, Wu JY, Thompson MJ, et al. Bone Health Management After Hematopoietic Cell Transplantation: An Expert Panel Opinion from the American Society for Transplantation and Cellular Therapy. Biol. Blood Marrow Transplant. 2020; 26: 1784-802.
2.Majhail NS, Rizzo JD, Lee SJ, Aljurf M, Atsuta Y, Bonfim C, et al. Recommended screening and preventive practices for long-term survivors after hematopoietic cell transplantation. Bone Marrow Transplant. 2012; 47: 337-41.
3.Schulte CM, Beelen DW. Bone loss following hematopoietic stem cell transplantation: a long-term follow-up. Blood. 2004; 103: 3635-43.
4.McClune BL, Polgreen LE, Burmeister LA, Blaes AH, Mulrooney DA, Burns LJ, et al. Screening, prevention and management of osteoporosis and bone loss in adult and pediatric hematopoietic cell transplant recipients. Bone Marrow Transplant. 2011; 46: 1-9.
5.Yao S, McCarthy PL, Dunford LM, Roy DM, Brown K, Paplham P, et al. High prevalence of early-onset osteopenia/osteoporosis after allogeneic stem cell transplantation and improvement after bisphosphonate therapy. Bone Marrow Transplant. 2008; 41: 393-8.
6.Pawlowska M, Yang Q, Hamata B, Kendler DL, Broady R. Early changes in bone mineral density and trabecular bone score following allogeneic stem cell transplant. Bone Marrow Transplant. 2016; 51: 738-40.
7.Kendler DL, Body JJ, Brandi ML, Broady R, Cannata-Andia J, Cannata-Ortiz MJ, et al. Bone management in hematologic stem cell transplant recipients. Osteoporos Int. 2018;29: 2597-610.
8.Population based reference standards of peak bone mineral density of Indian males and females: An ICMR multi-center task force study' 2010 NDIPPbD.,
9.Mithal A, Bansal B, Kyer CS, Ebeling P. The Asia-Pacific Regional Audit- Epidemiology, Costs, and Burden of Osteoporosis in India 2013: A report of International Osteoporosis Foundation. Indian J Endocrinol Metab. 2014; 18: 449-54.
10.Cherian KE, Kapoor N, Devasia AJ, Mathews V, Srivastava A, Thomas N, et al. Do Bone Density, Bone Microarchitecture, and Body Composition Differ in Recipients of Allogeneic Hematopoietic Stem Cell Transplant? A Cross-Sectional Study from Southern India. Biol. Blood Marrow Transplant. 2020; 26: 540-5.
11.Lewiecki EM, Binkley N, Morgan SL, Shuhart CR, Camargos BM, Carey JJ, et al. Best Practices for Dual-Energy Xray Absorptiometry Measurement and Reporting: International Society for Clinical Densitometry Guidance. J Clin Densitom. 2016; 19: 127-40.
12.ISCD. The International Society for Clinical Densitometry, 2019 ISCD Official Positions- Adult.
13.World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: report of a WHO study group [meeting held in Rome from 22 to 25 June 1992]. Geneva 1994.
14.Baumgartner A, Moesch M, Zumsteg M, Struja T, Bernet S, Medinger M, et al. Predictors of impaired bone health in long-term survivors after allogeneic stem cell transplantation. Bone Marrow Transplant. 2019; 54: 1651-61.
15.Limvorapitak W, Chernoff B, Lad D, Kendler D, Broady R. Changes in Bone Mineral Density and Bone Quality One Year Following Allogeneic Stem Cell Transplantation: Effects of Zoledronic Acid Infusion. Bone Marrow Transplant. 2018; 53: 307-9.
16.Kendler DL, Compston J, Carey JJ, Wu CH, Ibrahim A, Lewiecki EM. Repeating Measurement of Bone Mineral Density when Monitoring with Dual-energy X-ray Absorptiometry: 2019 ISCD Official Position. J Clin Densitom. 2019; 22: 489-500.
Search
News