Volume 2 (2019) Issue 4 No.2 Pages 54-57
Abstract
Hematopoietic stem cell transplantation (HSCT) was introduced in Myanmar in 2014 and was first performed in a patient with multiple myeloma at the North Okkalapa General and Teaching Hospital. From 2014 to 2016,transplantation activities were in the preliminary stage of establishing the infrastructure and gradually developing capacity-building. In 2016, the Yangon General Hospital also commenced autologous transplantation for myeloma. Five autologous transplants were performed in Myanmar during 2016 in patients with myeloma, using high-dose melphalan and non-cryopreserved peripheral blood stem cell rescue. Despite the lack of a National Registry system, all cases were reported in the activity survey due to their small number. The National Marrow Donor Program has not been implemented in Myanmar yet. The major limitation in promoting HSCT in Myanmar is the unavailability of health insurance coverage for blood and marrow transplantation (BMT). The patients who received transplantation were partly supported by the government and partly by their families through out-ofpocket expenses. However, despite limited resources, there has been substantial progress in the human resource development for BMT in Myanmar. Under the leadership of The Asia Pacific Blood and Marrow Transplantation Group (APBMT), several transplant centers in the Asia-Pacific region have been supporting Myanmar to establish transplantation activities and capacity-building for promoting HSCT in patients from Myanmar.
Current HSCT Activities in Myanmar
Hematopoietic stem cell transplantation (HSCT) was introduced in Myanmar in 2014. The first autologous stem cell transplantation (ASCT) was performed in a patient with multiple myeloma (MM) at the North Okkalapa General and Teaching Hospita (l NOGTH) in Yangon. From 2014 to 2016, transplantation activities were in the preliminary stage of establishing the infrastructure and gradually developing capacity-building. In 2016, the Yangon General Hospital (YGH) began ASCT for two patients with myeloma. Moreover, five ASCT were performed in 2016 at the two transplant centers in Yangon, the business capital of the country. From 2014 to 2016, only ASCT was performed for patients with MM in Myanmar using high-dose melphalan and non-cryopreserved peripheral blood stem cells (PBSCs) without mobilizing agents in a resource-limited setting. Despite facing resource constraints, the patients who received transplantation in 2014 remained in complete remission until the end of 2016, achieving an overall survival of one to two years.
National Registry in Myanmar
Despite the lack of a National Registry system, all cases were reported in the activity surveys of The Asia Pacific Blood and Marrow Transplantation Group (APBMT) and Worldwide Network for Blood & Marrow Transplantation (WBMT) due to their small number.
National Marrow Donor Program in Myanmar
Myanmar does not have a National Marrow Donor Program due to the absence of a bone marrow donor bank or cord blood bank. However, the National Blood Center (NBC) of Myanmar is planning to establish it in the future because of the lack of adequate resources at present.
Major Limitations in Promoting HSCT in Myanmar
The major limitation in promoting HSCT in Myanmar is the unavailability of health insurance coverage for blood and marrow transplantation (BMT). The transplant program is supported partly by the government and partly by the patients’ families. While essential drugs are subsidized by the government, most of the out-of-pocket expenses were incurred on laboratory tests at overseas institutions. Although essential laboratory tests are available locally, the assessment of minimal residual disease and tests for fungal and viral infection, such as the galactomannan test and CMV viral load, were performed at overseas laboratories, which accounted for a significant proportion of the patients’ out-of-pocket expenses. Inadequate human resources is a major problem in addition to the lack of specialized laboratory facilities. The hematologists leading the transplant team are also experiencing a high burden of malignant and non-malignant hematology cases, while oncologists are overburdened with a high number of solid tumor cases. Moreover, there is a shortage of nurses in the hematooncology, BMT, and critical care units, as the majority are laboratory technicians. Experienced hematopathologists, microbiologists or infectious disease specialists, and intensivists required for supportive care of transplant patients are lacking. The availability of drugs is another challenge because several drugs used during the transplant procedure were not registered due to their small purchase volume. Therefore, patients were administered single-use drugs, which were expensive and infrequently available. The emergence of drug-resistant bacteria and fungi is also a potential problem.
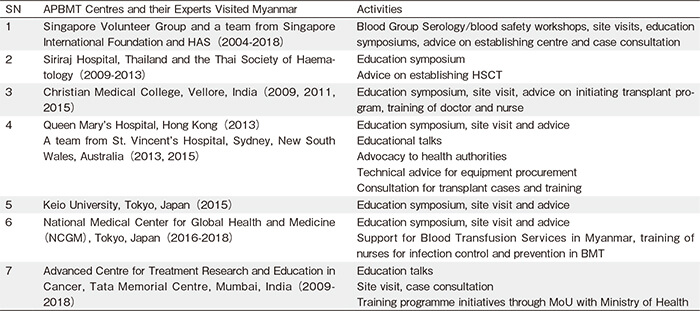
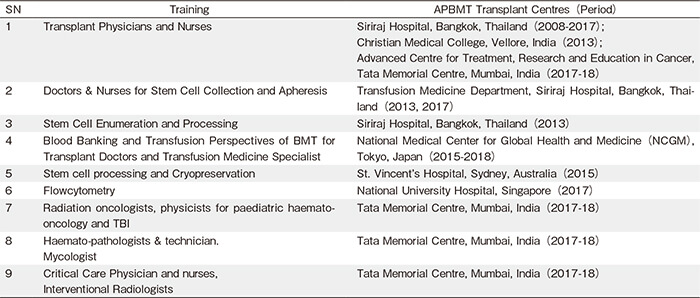
National Collaboration in the Past for Human Resource Development
Under the leadership of APBMT, several transplant centers from the Asia-Pacific region have been helping Myanmar to establish transplant activity and capacitybuilding. Since 2004, teams of transplant physicians from several transplant centers across the Asia-Pacific region have visited Myanmar and provided invaluable advice on developing infrastructure, selection of cases, development of transfusion and other laboratory support, and training doctors, nurses, and technicians to enable transplant activities in Myanmar. Teams from the Singapore Volunteer Group, Singapore International Foundation and Health Authority (2004-2017), Siriraj Hospital, Bangkok, Thailand, the Thai Society of Haematology (2009-2013), Christian Medical College, Vellore, India (2013), St. Vincent’s Hospital, Sydney, New South Wales, Australia (2013), Keio University (2013), Queen Mary’s Hospital, Hong Kong (2015), National Medical Center for Global Health and Medicine (NCGM), Tokyo, Japan (2015-2018), and Advanced Centre for Treatment Research and Education in Cancer, Tata Memorial Centre, Mumbai, India (2009–2018) have provided immense support (Table 1). Clinical training for doctors and nurses from the transplant units, intensive care units, and pediatric hematooncology units; transfusion and blood bank training, including apheresis collection of stem cells; laboratory training related to stem cell enumeration and flow cytometry; cell processing and cryopreservation; hematopathology and mycology; radiation oncology, and interventional radiology, were also provided at the centers shown in Table 2.
With such support, Myanmar developed the capacity to perform ASCT in 2017, thereby making HSCT a reality for patients in Myanmar1.
Future Strategies
Although financial constraints are a major obstacle for the expansion of transplant activities in Myanmar, there is still hope for a better future. Under Universal Health Coverage (UHC)-a strategy of the United Nations and World Health Organization aimed to provide essential health care as a global health priority-the Myanmar government has committed to attain universal health coverage by 20302. However, to prevent financial catastrophe resulting from out-of-pocket expenses, health insurance systems such as the government-organized national insurance system or social health insurance finance by income tax, which have been practiced in neighboring countries like China, Thailand, and Vietnam, can be viable option3,4. Despite the existence of the social security system in Myanmar, its coverage is limited to individuals from selected government ministries and public sector employees. Until the adequate development of such systems is achieved, transplant activities in Myanmar would primarily depend on government support under the Ministry of Health and Sports for drugs, equipment, and consumables. Human resource development will be continued by training health professionals locally by conducting local training courses, expanding academic collaboration between centers from neighboring countries to organize twinning programs, and increasing support and collaboration from professional societies such as the American Society of Hematology. The construction of a central laboratory service has been initiated as planned and capacity- building for laboratory personnel has been organized with support from neighboring countries, although many remain to be covered.
Conclusion
Although a small step for APBMT, the establishment of HSCT in Myanmar under resource constraint has become a reality for patients in Myanmar. However, further effort needs to be undertaken to ensure robust development.
Acknowledgements
The authors would like to acknowledge the following experts from APBMT for their contribution in the establishment of the BMT and human resource development in Myanmar:
・ Professor Mammen CHANDY, Christian Medical College,Vellore, India
・ Professor James CHIM, University of Hong Kong,Hong Kong
・ Professor Anthony DODDS, St. Vincent’s Hospital,Sydney, New South Wales, Australia
・ Dr. S. HAGIWARA, National Medical Center for Global Health and Medicine (NCGM), Tokyo, Japan (2015-2018)
・ Professor Navin KHATTRY, Advanced Centre for Treatment Research and Education in Cancer, Tata Memorial Centre, Mumbai, India
・ Professor Yoshihira KODERA, WBMT/APBMT
・ Professor Mickey KOH, Singapore Volunteer Group,Singapore International Foundation and and Director,Stem Cell Transplantation at St George’s Hospital and Medical School, London, UK
・ Professor David MA, St. Vincent’s Hospital, Sydney,New South Wales, Australia
・ Professor Vikram MATHEWS, Christian Medical College,Vellore, India
・ Professor Surapol ISSARAGRISIL, Siriraj Hospital,Thailand
・ Professor Shinichiro OKAMOTO, Keio University,Tokyo, Japan
・ Professor Tapan SAIKIA, Tata Memorial Centre,Mumbai, India
・ Professor Alok SRIVASTAVA, Christian Medical College,Vellore, India
Authors’ Contribution
A. A. G. and H. L. N. led the transplant teams and T. D. A. was responsible for transfusion medicine part of transplant. R. M. was involved in capacity building. With contribution from all authors, A. A. G. wrote the manuscript.
Conflict of Interest
The authors declare no conflict of interest. Disclosure forms provided by the authors are available here.
References
1. Gyi AA, Mra R, Nyein HL, Aung T, Win N, Khin PT, et al. Where there’s a will, there’s a way: establishing haematopoietic stem cell transplantation in Myanmar. Blood Advances. 2017; Special Annual Meeting edition: 125-9.
2. Han SM, Rahman MM, Rahman MS, Swe KT, Palmer M, Sakamoto H, et al. Progress towards universal health coverage in Myanmar: a national and subnational assessment. The Lancet Public Health. 2018; 6: e989-97.
3. Meng Q, Xu L, Zhang Y, Qian J, Cai M, Xin Y, et al. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet. 2012; 379: 805-14.
4. Tangcharoensathien V, Patcharanarumol W, Ir P, Syed Junid SMA-J, Mukti AG, Akkhavong K, et al. Health-financing reforms in southeast Asia: challenges in achieving universal coverage. Lancet. 2011; 377: 863-73.
Search
News



